BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://jsurgery.bums.ac.ir/article-1-157-en.html
Evaluation of relationship between presbyopia and presbycusis in Vali-e-Asr Hospital in Birjand, Iran, during 2014-2015
Ghasem Karimi1, Mohammad Hossein Davari2*, Vahid Ghorriani3
1Associate Professor, Department of Ear, Nose, and Throat surgery, Faculty of Medicine, Birjand University of Medical Sciences, Birjand, Iran
2Assistant Professor, Department of Ophthalmology, Cardiovascular Disease Research Center, Birjand University of Medical Sciences, Birjand, Iran
3Student Research Committee, Cardiovascular Disease Research Center, Birjand University of Medical Sciences, Birjand, Iran
Received: June 04, 2018 Revised: December 01, 2018 Accepted: December 02, 2018
|
Abstract Introduction: Presbyopia and presbycusis are common disorders in aging people leading to various negative consequences, such as social problems, cognitive disorders, depression, and imbalance. The combination of vision and hearing loss has been correlated with various adverse outcomes. Regarding the adverse effect of presbyopia and presbycusis on communication skills and quality of life in individuals, this study was conducted to determine the relationship between these two sensory disorders. Methods: This cross-sectional study was performed on 111 patients with presbyopia referred to Ophthalmology Clinic of Vali-e-Asr Hospital in Birjand, Iran, from 1395 to 1396. The patients who met reduced visual acuity criteria were included in the study. On the other hand, the exclusion criteria were: 1) diabetes, 2) glaucoma, 3) ear infection disease, 4) kidney disease, 5) history of head injury, 6) history of ototoxicity, 7) history of ear and intracranial tumors, and 8) experience of working in noisy environments. Presbyopia and presbycusis were diagnosed with routine clinical examinations. The data were analyzed in SPSS software (Version 22.0) using the Chi-square, Fisher's exact, and Mann-Whitney U tests. Results: The results of the study showed that 70%, 64%, and 55% of the patients in the age ranges of 45-49, 50-55, and Conclusions: There was no relationship between presbyopia and presbycusis. The incidence of presbyopia was more than 50% and mild hearing impairment was observed in patients. In addition, the treatment of these disorders can prevent adverse consequences, such as cognitive impairment and falling down. Key words: Hearing loss, Presbycusis, Presbyopia |
Introduction
Presbyopia is the normal loss of near focusing ability that occurs particularly with age. It appears due to the gradual thickening and loss of flexibility of the natural lens inside the eye. These age-related changes occur within the proteins in the lens, making the lens harder and less elastic over time (1). Age-related changes also take place in the muscle fibers surrounding the lens (2). With less elasticity, the eye has a harder time focusing up close. In fact, the word "presbyopia" means "old eye" in Greek. Most people begin to notice the effects of presbyopia sometime after age 40, when they start having trouble seeing clearly small prints, including books, magazines, and text messages on their phone (3, 4).
Generally, a series of irreversible changes in the body is due to aging, and presbyopia is one of these changes. Presbyopia is not a worrying problem and can be easily treated. In order to create a clear image of an object on the retina, it should do its job of concentrating light structures, such as the cornea and lens.
In contrast to the cornea, the lens is more flexible. With the increase of its thickness to see close objects, it focuses more on the light beams so that the image of the object is clearly created on the retina. This change in thickness is caused by special intraocular muscle contraction. As the age increases, changes in the eyes occur and the hardening of the lens leads to presbyopia. When the lens loses its flexibility, it cannot change the thickness so it will not be able to optimally concentrate the light rays resulting from the objects. Therefore, the resulting images will become blurred (1).
Risk factors that have been identified for presbyopia include hyperopia requiring great lens flexibility, patient's career especially if it requires near vision, eye disease, trauma, and damage to lenses or muscles which accelerate the progression of presbyopia.
Systemic diseases, such as diabetes, multiple sclerosis can also expose the patient to presbyopia. Moreover, drink and drug consumption, including alcohol, antidepressants, and antihistamines can reduce the lens's flexibility. The other risk factors are geographical ones, such as high annual temperature, high exposure to ultraviolet radiation, and people living near the equatorial line (1, 2).This disorder is detectable by performing basic clinical examinations of the eye, and the diagnosis is usually done by a specialist. In addition to the diagnosis, the specialist can also recommend the necessary treatment.
Prevalence rate of presbyopia in Africa was reported to rise by 85% in 400 patients aged 40 to 50 years old (5). In the study of Akhgari et al. in Tehran, 41% and 90% of the patients with presbyopia were over 90 and 40 years old, respectively (6). In the study of Burke et al., the prevalence of this disorder was about 60%, which had a direct relationship with age, female gender, higher education level and urban life (7). This disease has significantly reduced the quality of life of the patients. Due to the high prevalence of this disorder, it affects the quality of the life of a large part of society (2, 6, 8).
Another disorder that has a significant prevalence in the middle-aged and aged people is hearing loss and presbycusis disorder. Various studies have shown that presbycusis is the common disorder in people over 60 years and older (9-12). Hearing loss is the most common elderly disorder recorded in ear, throat and nose department (13).
This kind of symmetric sensory nervous disorder is a disease associated with age in people over 50 years. With aging, the nerve cells of the inner ear, which are responsible for converting sound to an electrical current, become as weak as the other components of the body. It is obvious that with the weakening of these cells, the level of hearing of the individual will be reduced. The hearing impairment in people with presbycusis is usually progressive and bilateral, and both ears are almost equally affected by hearing loss. Due to the gradual progression of presbycusis, the person who has suffered from this disorder may not perceive a reduction in his hearing for a long time. Hearing loss in people who suffer from presbycusis is not the same at all frequencies, however, these people usually encounter more troubles hearing the higher frequency sounds.
These people have difficulties in hearing the nearby phone ring, while it's possible to hear the sound of a car running on the street. Normally, people who are suffering from presbycusis can hear sounds slower and more obscure. These people may hear the sound; however, they have trouble in distinguishing the words from each other. For instance, they hear the word "zang" instead of "nang". Clinical manifestations of this disorder are in the form of bilateral deafness, which occurs initially in high tones and later in moderate frequencies. Gradually, the patient experiences Social deafness so that he is no longer able to take part in multiplayer conversation (14). The prevalence of this impairment has been different in various communities and according to studies done it has a remarkable prevalence in Iran (15-17).
The age of hearing loss prevalence and the rate of its progress depend on several factors, most important of which is genetic predisposition. Nutrition and metabolism and the amount of noise pollution in the living environment are also factors that affect the presbycusis. Moreover, factors that reduce blood supply to inner ear can also accelerate the damage to ear sensitive cells; therefore, heart disease, high blood pressure, and diabetes can also cause premature presbycusis. This disease also reduce the quality of life patients significantly (18, 19). The term "dual sensory impairment" is used to refer to individuals suffering from both hearing and vision impairments (20, 21).
Presbyopia and presbycusis are of high prevalence at middle-aged and aged people, both of which decrease the quality of life of this group of patients (6, 8, 18, 19). Given this background
in mind, this important case has attracted researchers’ attention more than ever to evaluate the simultaneous occurrence of these two diseases in elderly people. Furthermore, several studies have been conducted to develop diagnostic protocols, algorithms, and clinical guidelines for concurrent treatment of both disorders (24-22).
According to the available literature, no studies have been carried out so far on the investigation of relation between presbyopia and presbycusis in Iran. Moreover, the adverse effects of presbycusis and presbyopia on the communication skills and quality of individuals’ life have been observed in several studies. To this end, the present study aimed to assess the prevalence of presbycusis in presbyopic patients referring to Ophthalmology Clinic of Vali-e-Asr Hospital in Birjand, Iran.
Methods
This descriptive-analytical study was performed on 111 presbyopic patients referring to Ophthalmology Clinic of Vali-e-Asr Hospital in Birjand, Iran from 1395 to 1396. All patients were examined using a slide lamp and other ophthalmic examinations. After assessing and determining the presbyopia, they were referred to the ear, nose and throat clinic and were also subjected to hearing tests. Before the implementation of the design, the study protocol was approved by the Ethics Committee of Birjand University of Medical Sciences, Birjand, Iran (IR.Bums.REC.1395.63).
The required criterion for the prevalence of presbyopia was numbers on eyeglass prescription. The patients whose spectacles were with convex lenses were regarded as presbyopic. All stages of examination, interpretation, and decision-making processes for patients were performed by an ophthalmologist.
Early diagnosis of presbycusis was based on history, clinical examination, and with the confirmation of earing measurement teat (Ear Tape). A pure audiometric test was used to assess hearing loss based on the latest presbycusis diagnostic criteria (see appendix). The interpretation of the test results and the performance of all cases were done by an expert. Sampling was done using a pink manner to be distributed to a proportion of patients in any age group of 45-50, 50-55, and 55- 60 years old.
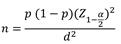
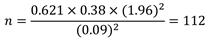
Based on the findings of a study conducted by Schneider et al. (21), and considering P=0.621 and d=0.09, the required sample size was obtained as 110 people according to the following formula; however, 111 patients with presbyopia were included in the study for evaluation.
The patients who met reduced visual acuity criteria were included in the study. On the other hand, the exclusion criteria were: 1) diabetes, 2) glaucoma, 3) ear infection disease, 4) renal disease, 5) history of head injury, 6) history of ototoxicity, 7) history of ear and intracranial tumors, and 8) experience of working in noisy environments.
The demographic features of the patients, such as age, gender, the presence and type of cataracts, and drug, cigarettes, and alcohol consumption were collected. The data were analyzed in SPSS (version 22.0) using the Chi-square, Fisher's exact, and Mann-Whitney U tests. P-value of ≤0.05 was considered to be statistically significant.
Results
Out of 111 participants, 58.6% of the cases were female and 79.1% of the respondents were born in city. With regard to the employment status, 45%, 14.7%, 21.1%, 10.1%, and 9.1% of the subjects were housewives, retired, workers
and farmers, self-employed, and employees, respectively. No vision problems was observed in 30%, 36%, and 45% of the patients in three age groups of 45-49, 50-55, and 56-60, respectively.
There was no relationship between vision problem and age groups. However, 30.6%, 4.7%, 13.5%, and 6.3% of the patients were affected with myopic and hyperopic astigmatism, myopia, and hyperopia, respectively. The right and left eyes were prescribed -1.00 in 71.2% and 68.5% of the participants, respectively. There was no significant correlation between the eye prescription numbers and the age group.
Table1: Central indicators and dispersion of visual acuity and hearing
|
Maximum |
Minimum
|
Mean (±std) |
|
|
80 |
6.60 |
20.31 (±11.49) |
Hearing ability (right ear) |
|
75 |
6.60 |
20.06 (±12.19) |
Hearing ability (left ear) |
|
13 |
0 |
1.68 (±2.06) |
Numbers on eyeglass prescription (right eye) |
|
13 |
0 |
1.68 (±2.01) |
Numbers on eyeglass prescription (left eye) |
Table 2: Distribution of percentage of right and left presbycusis by demographic variables
|
P-value |
Left Presbycusis |
P-value |
Right Presbycusis |
Variables |
|||||||
|
Sever |
Moderate |
Mild |
Normal |
Sever |
Moderate |
Mild |
Normal |
||||
|
0.22 |
0 |
1 (50) |
17 (53.1) |
28 (37.8) |
0.76 |
2 (66.7) |
1 (25) |
17 (43.6) |
26 (40) |
Male |
Gender |
|
3 (100) |
1 (500 |
15 (46.9) |
46 (62.2) |
1 (33.3) |
3 (75) |
22 (56.4) |
39 (60) |
Female |
|||
|
0.62 |
3 (100) |
2 (100) |
23 (71.9) |
59 (80.8) |
0.07 |
3 (100) |
3 (75) |
25 (65.8) |
56 (86.2) |
Urban |
Place of residence |
|
0 |
0 |
9 (28.1) |
14 (19.2) |
0 |
1 (25) |
13 (34.2) |
9 (13.8) |
Rural |
|||
|
0.16 |
0 |
0 |
9 (28.1) |
28 (37.8) |
0.50 |
0 |
1 (25) |
12 (30.8) |
24 (36.9) |
45-49 |
Age group |
|
1 (33.3) |
1 (50) |
8 (25) |
27 (36.5) |
0 |
2 (50) |
14 (35.9) |
21 (32.3) |
50-55 |
|||
|
2 (66.7) |
1 (50) |
15 (46.9) |
19 (25.7) |
3 (100) |
1 (25) |
13 (33.3) |
20 (30.8) |
56-60 |
|||
Table3: Comparison of presbycusis in right and left eye
|
Left eye mean (±std) |
Right eye mean (±std) |
|
|
|
1.02 (±1.95) |
1.02 (±1.97) |
Normal |
Presbycusis (Right ear) |
|
0.79 (±1.30) |
0.78 (±1.36) |
Abnormal |
|
|
0.62 |
0.68 |
P-value (Mann-Whitney) |
|
|
1.07 (±1.95) |
1.04 (±1.95) |
Normal |
Presbycusis (Left ear) |
|
0.62 (±1.02) |
0.69 (±1.22) |
Abnormal |
|
|
0.35 |
0.42 |
P-value (Mann-Whitney) |
|
Normal hearing ranges from 0 to 20 decibels (db) in all frequencies and the means of right and left ear hearing ability in the respondents were obtained as 20.31 (±11.49) and 20.06 (±12.19) db, respectively. Therefore, the observed results indicated that the respondents had moderate hearing impairment. With respect to the right ear, %58.56 of the respondents had normal hearing, whereas 41.44 % of the cases had moderate hearing loss. On the other hand, 66.67 % of the patients had normal hearing, while 33.33 % of the subjects were affected with moderate hearing loss in the left ear.
The mean ages of the onset of the presbycusis in the right and left ears were 53.22 ± 5.64 and 54.16 ± 5.61 years, respectively. Accordingly, there was no significant correlation between right and left ear presbycusis and gender, age group, and place of residence (i.e., rural, urban)
The numbers on eyeglass prescription of the right and left eyes of the respondents were 1.68 ± 2.6 and 1.68 ± 2.01, respectively. In order to determine the relationship between hearing loss and visual acuity, Fisher's correlation test was used. The results showed that there was no significant correlation between hearing abilities and numbers on eyeglass prescription. In addition, according to the results of the Mann-Whitney test, there was no significant differences between the mean score of numbers on eyeglass prescription and the severity of presbycusis.
Discussion
The study purpose was to determine the prevalence of presbyopia and presbycusis in aging patients referring to Ophthalmology Clinic of Vali-e-Asr Hospital in Birjand, Iran. It was also aimed to investigate the relationship between these two sensory disorders. The results of the study showed that 70%, 64%, and 55% of the patients in three age groups of 45-49, 50-55, and 56- 60 had different vision problems and mild hearing impairment, respectively.
According to the results, there was no correlation between presbyopia and presbycusis in terms of gender and place of residence (i.e., rural, urban). No relationship was also observed between these two sensory impairments. There are controversies in literature regarding the prevalence of presbyopia and presbycusis in aging people. In a study conducted by Grow et al. on 770 elderly subjects, 48% and 32% of the patients were affected by presbycusis and presbyopia, respectively. Moreover, 20% of the cases suffered from hearing and vision impairments leading to balance disorders, such as falling down (25).In the Heidi study, the incidence of presbyopia among the elderly was reported to be 80% (3). In another study performed on 625 elderly patients, the prevalence rate of presbycusis was obtained as 36.1%. The variables, such as age, gender, diabetes, and hereditary hearing impairment were recognized as risk factors; however, there was no relation between cardiovascular disease, smoking, and alcohol consumption and the incidence of presbyopia (26). Chang et al. showed the prevalence of presbycusis in four age groups of 65-69, 70-74, 75-79, and over 80 as 1.6%, 3.2%, 7.5%, and 14.9%, respectively (27). In another study, 25.4% and 45% of the elderly patients were affected by visual and hearing impairment, respectively. Moreover, 15.1% of the cases suffered from both disorders (22). In a study carried out by Jay et al., it was reported that 30.2% and 50.5% of the elderly had visual and hearing impairments, respectively. In addition, 22.5% of the patients were affected by presbyopia and presbycusis (28). Furthermore, Schneider et al. showed the prevalence of vision and hearing impairments in 13% and 10% of the aged patients. They also found that 5% of the elderly suffered from both visual and hearing impairments (21).
Presbyopia and presbycusis have many negative effects on individuals' personal and social lives, such as social isolation, cognitive impairment, depression, and imbalance. Moreover, the combination of vision and hearing loss has been correlated with various adverse outcomes. In another study, it has been reported that older people affected by vision and hearing impairment encountered a lot of problems, two of which were social isolation and the limitation of social activities (29).
According to the literature, there was no correlation between hearing impairment in elderly people over 69 years old and cognitive and functional impairment. However, an association was observed between visual impairment and cognitive and functional disorders in elderly patients. A significant association was also observed between these two disorders and cognitive and functional impairment which was more prevalent in older females. It has been reported that the treatment of hearing and vision impairments is probably reduce the risk of cognitive and functional decline among the elderly (30). A study investigated the effect of gender and age range of 76-81 years on visual and hearing impairments. The result showed that the visual and hearing impairments were prevalent in females and males, respectively. There was also an association between visual and hearing impairments and the increased risk of falling down and injuries.
However, no significant difference was reported with regard to the relation between gender and the risk of imbalance and falling own (31). Chou et al., showed that vision and hearing impairments had a direct relationship with depression which was more prevalent in presbyopic patients (32).With regard to the high prevalence of presbyopia and presbycusis and their adverse consequences on the individuals' personal and social lives, preventive measures should be taken in to account. Timely treatment and the risk alleviation of these disorders in aging people lead to the reduction of cognitive impairment, depression, imbalance, and other social problems.
In a study conducted by Saroj B, Raj K, et al., presbyopia and presbycusis were indicated to increase gradually with the age; however, no relationship was found between these two disorders and variables, such as arterial hypertension, blood sugar level, serum cholesterol level, and the consumption of tobacco (33).
Conclusions
There was no association between presbyopia and presbycusis. The incidence of presbyopia was more than 50% and mild hearing impairment was observed in all patients. In addition, the treatment of these disorders can prevent negative consequences, such as cognitive impairment and falling down.
Acknowledgments
This article was derived from a thesis by Dr. Vahid Ghorriani, supervised by Dr. Ghasem Karimi, and advised by Dr. Mohammad Hossein Davari. The authors of this study would like to thank all colleagues in the Ophthalmology Department and Clinical Research Center of Vali-e-Asr Hospital in Birjand. We also acknowledge Mrs. Monirah Sannaei for her kind help in conducting the research.
Author’s contribution
Dr. Mohammad Hossein Davari conducted the analysis, designed and monitored the study, wrote the manuscript, and carried out the final edition. Dr. Ghasem Karimi performed data collection and edited the article. Dr. Vahid Ghoriani, monitored the plan, edited the manuscript, and translated the article in to English.
Funding
No funding is received from a known resource.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of the study.
References
1. Nirmalan PK, Krishnaiah S, Shamanna BR, Rao GN, Thomas R. A population-based assessment of presbyopia in the state of Andhra Pradesh, south India: the andhra pradesh eye disease study. Invest Ophthalmol Vis Sci. 2006; 47(6):2324-8. PMID: 16723440 DOI: 10.1167/iovs.05-1192
2. Patel I, Munoz B, Burke AG, Kayongoya A, Mchiwa W, Schwarzwalder AW, et al. Impact of presbyopia on quality of life in a rural African setting. Ophthalmology. 2006; 113(5):728-34. PMID: 16650665 DOI: 10.1016/j.ophtha.2006.01.028
3. Laviers H. The prevalence of presbyopia and the feasibility of community distribution of near spectacles in adults in Zanzibar, East Africa. Community Eye Health. 2007; 20(64):73. PMID: 18330449
4. Akhgary M, Ghassemi BM, Aghazadeh AM, Tabatabaee SM, Khosravi B. The prevalence of anisometropia in patients examined in optometry clinic of rehabilitation Faculty of Shahid Beheshti Medical University. Sci J Rehabil Med. 2013; 2(3):39-44.
5. Abrahamson JI. Eye changes after forty. Am Family Phys. 1984; 29(4):171-81. PMID: 6720493
6. Weale RA. Epidemiology of refractive errors and presbyopia. Surv Ophthalmol. 2003; 48(5):515-43. PMID: 14499819
7. Burke AG, Patel I, Munoz B, Kayongoya A, Mchiwa W, Schwarzwalder AW, et al. Population-based study of presbyopia in rural Tanzania. Ophthalmology. 2006; 113(5):723-7. PMID: 16650664 DOI: 10.1016/
j.ophtha.2006.01.030
8. Gates GA, Caspary DM, Clark W, Pillsbury HC 3rd, Brown SC, Dobie RA. Presbycusis. Otolaryngol Head Neck Surg. 1989; 100(4):266-71. PMID: 2498811 DOI: 10.1177/019459988910000403
9. Mazelová J, Popelar J, Syka J. Auditory function in presbycusis: peripheral vs. central changes. Exp Gerontol. 2003; 38(1):87-94. PMID: 12543265
10. Gates GA, Cooper JC. Incidence of hearing decline in the elderly. Acta Otolaryngol. 1991; 111(2):240-8. PMID: 2068909
11. Gates GA, Cooper JC Jr, Kannel WB, Miller NJ. Hearing in the elderly: the framingham cohort, 1983-1985. Part 1. Basic audiometric test results. Ear Hear. 1990; 11(4):247-56. PMID: 2210098
12. Takeda S, Morioka I, Miyashita K, Okumura A, Yoshida Y, Matsumoto K. Age variation in the upper limit of hearing. Eur J Appl Physiol Occup Physiol. 1992; 65(5):403-8. PMID: 1425644
13. Calhoun KH, Eibling DE. Geriatric otolaryngology. Florida: CRC Press; 2006.
14. Behrbohm H, Kaschke O. Ear, nose, and throat diseases: with head and neck surgery. Stuttgart, Germany: Thieme; 2009.
15. Yagana Moghadam A, Jafari H, Ghorbani M, Dalirian A. Prevalence evaluation of hearing loss on referral to audiology clinic of Matini hospital 2006. Feyz. 2007; 10:61-7.
16. Jafari Z, Malayeri S, Rashedi P. Effects of age on the auditory system and process of presbycusis in the audiology centers of Tehran. Salmand. 2007; 2(3):358-64.
17. Cruickshanks KJ, Wiley TL, Tweed TS, Klein BE, Klein R, Mares-Perlman JA, et al. Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin: the epidemiology of hearing loss study. Am J Epidemiol. 1998; 148(9):879-86. PMID: 9801018
18. Ciorba A, Bianchini C, Pelucchi S, Pastore A. The impact of hearing loss on the quality of life of elderly adults. Clin Interv Aging. 2012; 7:159-63. PMID: 22791988 DOI: 10.2147/CIA.S26059
19. Li-Korotky HS. Age-related hearing loss: quality of care for quality of life. Gerontologist. 2012; 52(2):265-71. PMID: 22383543 DOI: 10.1093/
geront/gnr159
20. Saunders GH, Echt K. Dual sensory impairment in an aging population. ASHA Leader. 2011; 16(3):5-7. DOI:10.1044/leader.FTR4.16032011.5
21. Schneider JM, McMahon CM, Gopinath B, Kifley A, Barton R, Mitchell P, et al. Dual sensory impairment and hearing aid use among clients attending low-vision services in Australia: The vision-hearing project. J Aging Health. 2014; 26(2):231-49. PMID: 24344196 DOI: 10.1177/0898264313513610
22. Schneck ME, Lott LA, Haegerstrom‐Portnoy G, Brabyn JA. Association between hearing and vision impairments in older adults. Ophthalmic Physiol
Opt. 2012; 32(1):45-52. PMID: 21999724 DOI: 10.1111/j.1475-1313.2011.00876.x
23. Klein BE, Cruickshanks KJ, Nondahl DM, Klein R, Dalton DS. Cataract and hearing loss in a population-based study: the Beaver Dam studies. Am J Ophthalmol. 2001; 132(4):537-43. PMID: 11589876
24. Vreeken HL, van Rens GH, Kramer SE, Knol DL, Festen JM, van Nispen RM. Dual sensory loss: development of a dual sensory loss protocol and design of a randomized controlled trial. BMC Geriatr. 2013; 13(1):84. PMID: 23941667 DOI: 10.1186/1471-2318-13-84
25. Grue EV, Ranhoff AH, Noro A, Finne‐Soveri H, Jensdóttir AB, Ljunggren G, et al. Vision and hearing impairments and their associations with falling and loss of instrumental activities in daily living in acute hospitalized older persons in five Nordic hospitals. Scand J Caring Sci. 2009; 23(4):635-43. PMID: 19068040 DOI: 10.1111/j.1471-6712.2008.00654.x
26. Sousa CS, Castro Junior N, Larsson EJ, Ching TH. Risk factors for presbycusis in a socio-economic middle-class sample. Braz J Otorhinolaryngol. 2009; 75(4):
530-6. PMID: 19784422
27. Chang HP, Chou P. Presbycusis among older Chinese people in Taipei, Taiwan: a community-based study. Int J Audiol. 2007; 46(12):738-45. PMID: 18049963 DOI: 10.1080/14992020701558529
28. Jee J, Wang JJ, Rose KA, Lindley R, Landau P, Mitchell P. Vision and hearing impairment in aged care clients. Ophthalmic Epidemiol. 2005; 12(3):199-205. PMID: 16036479 DOI: 10.1080/09286580590969707
29. Crews JE, Campbell VA. Vision impairment and hearing loss among community-dwelling older Americans: implications for health and functioning. Am J Public Health. 2004; 94(5):823-9. PMID: 15117707
30. Lin MY, Gutierrez PR, Stone KL, Yaffe K, Ensrud KE, Fink HA, et al. Vision impairment and combined vision and hearing impairment predict cognitive and functional decline in older women. J Am Geriatr Soc. 2004; 52(12):1996-2002. PMID: 15571533 DOI: 10.1111/j.1532-5415.2004.52554.x
31. Lopez D, McCaul KA, Hankey GJ, Norman PE, Almeida OP, Dobson AJ, et al. Falls, injuries from falls, health related quality of life and mortality in older adults with vision and hearing impairment--is there a gender difference? Maturitas. 2011; 69(4):359-64. PMID: 21664773 DOI: 10.1016/j.maturitas.2011.
05.006
32. Chou KL, Chi I. Combined effect of vision and hearing impairment on depression in elderly Chinese. Int
J Geriatr Psychiatry. 2004; 19(9):825-32. PMID: 15352139 DOI: 10.1002/gps.1174
33. Bala S, Kumar R, Kaur I, Singh J, Kaur P, Sharma S. Evaluation of demographic profile of patients with presbyopia and presbycusis. J Adv Med Dent Sci Res. 2016; 4(4):10. DOI:10.21276/jamdsr.2016.4.4.3
Received: 2018/06/4 | Accepted: 2018/12/2 | ePublished ahead of print: 2018/12/24 | Published: 2018/12/24
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |









