Volume 13, Issue 1 (2-2025)
J Surg Trauma 2025, 13(1): 35-38 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Khani-Eshratabadi M, Salati S, Tashakori A, Ghaemi M, Kheradmand D. Non-invasive Management of Ventriculoperitoneal Shunt Dysfunction: A Case Report on Tactile Stimulation as a Therapeutic Approach. J Surg Trauma 2025; 13 (1) :35-38
URL: http://jsurgery.bums.ac.ir/article-1-458-en.html
URL: http://jsurgery.bums.ac.ir/article-1-458-en.html
Department of Neurosurgery, Birjand University of Medical Sciences, Birjand, Iran
Full-Text [PDF 355 kb]
(625 Downloads)
| Abstract (HTML) (2483 Views)
Full-Text: (640 Views)
Abstract
Hydrocephalus is a neurological disorder characterized by the abnormal accumulation of cerebrospinal fluid in the brain ventricles, which can cause increased intracranial pressure and damage to brain tissue. Surgical intervention, particularly ventriculoperitoneal (VP) shunt placement, is the mainstay of treatment for hydrocephalus; however, it is associated with complications, such as infection, blockage, and malfunction. This case report presents a non-surgical approach for the treatment of VP shunt dysfunction through regular tactile stimulation of the shunt pump. A 40-year-old female patient with a calcified VP shunt, originally placed in infancy, presented with symptoms of shunt dysfunction. Instead of surgical replacement, the patient was advised to perform a tactile regimen consisting of fifteen massages per day on the shunt pump. After 10 days of this intervention, the patient showed significant improvement in symptoms, and no shunt-related complications were observed during the six-month follow-up period. This case highlights the potential benefits of non-invasive interventions for VP shunt dysfunction, particularly in cases where traditional surgical methods may pose significant risks. However, the findings are limited to a single case, and further research is necessary to assess the safety and effectiveness of this approach before it can be widely adopted as a treatment option.
Key words: Complications, Hydrocephalus, Ventriculoperitoneal Shunt
Hydrocephalus is a neurological disorder characterized by the abnormal accumulation of cerebrospinal fluid in the brain ventricles, which can cause increased intracranial pressure and damage to brain tissue. Surgical intervention, particularly ventriculoperitoneal (VP) shunt placement, is the mainstay of treatment for hydrocephalus; however, it is associated with complications, such as infection, blockage, and malfunction. This case report presents a non-surgical approach for the treatment of VP shunt dysfunction through regular tactile stimulation of the shunt pump. A 40-year-old female patient with a calcified VP shunt, originally placed in infancy, presented with symptoms of shunt dysfunction. Instead of surgical replacement, the patient was advised to perform a tactile regimen consisting of fifteen massages per day on the shunt pump. After 10 days of this intervention, the patient showed significant improvement in symptoms, and no shunt-related complications were observed during the six-month follow-up period. This case highlights the potential benefits of non-invasive interventions for VP shunt dysfunction, particularly in cases where traditional surgical methods may pose significant risks. However, the findings are limited to a single case, and further research is necessary to assess the safety and effectiveness of this approach before it can be widely adopted as a treatment option.
Key words: Complications, Hydrocephalus, Ventriculoperitoneal Shunt
Introduction
Hydrocephalus is a prevalent neurosurgical disorder globally, marked by an abnormal accumulation of cerebrospinal fluid (CSF) within the brain's ventricles. Despite ongoing research efforts, the optimal treatment for hydrocephalus remains a topic of debate. The most commonly utilized intervention is ventriculoperitoneal (VP) shunt surgery, which involves implanting a shunt to divert CSF from the brain to the peritoneal cavity. While this procedure effectively alleviates symptoms, such as headaches, nausea, vomiting, and visual disturbances, it is not without risks. Shunt surgery can lead to complications, including malfunction, infection, blockage, and migration, which, if not promptly addressed, may result in severe neurological consequences. Furthermore, patients often face the need for repeated surgical interventions throughout their lives due to potential complications or changes in their clinical status (1,2).
In some instances, patients with existing shunts may avoid surgical replacements by employing more straightforward treatment strategies. For instance, one case highlighted a patient who had maintained a shunt for an extended period without requiring replacement. When symptoms eventually prompted a need for intervention, a novel nonsurgical approach was successfully implemented, yielding durable results without the necessity for revision surgery. This particular case underscores the potential benefits of alternative treatment options for hydrocephalus patients, particularly for those at high risk of complications from traditional surgical methods (3,4).
In light of these considerations, there is a growing need for alternative treatment modalities that can minimize the need for invasive procedures. One promising avenue is the theoretical basis for tactile stimulation of the shunt pump. This non-invasive approach aims to dislodge minor obstructions or enhance CSF flow through mechanical manipulation of the shunt. Although the exact mechanism remains unclear, it is hypothesized that regular massage of the shunt pump may help maintain its patency and functionality, particularly in cases involving partial obstruction or calcification (5,6).
This case report explores the application of the tactile stimulation method in a patient with a long-standing VP shunt, providing preliminary evidence of its viability as an alternative to surgical revision. By highlighting this non-invasive strategy, we hope to encourage further investigation into less invasive treatments that could significantly improve the quality of life for hydrocephalus patients.
Case
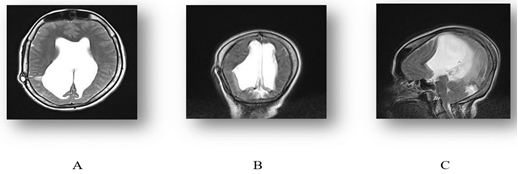
A 40-year-old female patient arrived at the emergency department of Abulfazl Hospital in Kashmar City, Iran, presenting with a variety of concerning symptoms, including severe headaches, hypertension, blurred vision, weakness, lethargy, nausea, and photophobia. Despite receiving supportive treatment and undergoing a thorough clinical examination, her symptoms did not improve, which prompted the attending physician to order both a brain CT scan and an MRI (Figure 1).
Hydrocephalus is a prevalent neurosurgical disorder globally, marked by an abnormal accumulation of cerebrospinal fluid (CSF) within the brain's ventricles. Despite ongoing research efforts, the optimal treatment for hydrocephalus remains a topic of debate. The most commonly utilized intervention is ventriculoperitoneal (VP) shunt surgery, which involves implanting a shunt to divert CSF from the brain to the peritoneal cavity. While this procedure effectively alleviates symptoms, such as headaches, nausea, vomiting, and visual disturbances, it is not without risks. Shunt surgery can lead to complications, including malfunction, infection, blockage, and migration, which, if not promptly addressed, may result in severe neurological consequences. Furthermore, patients often face the need for repeated surgical interventions throughout their lives due to potential complications or changes in their clinical status (1,2).
In some instances, patients with existing shunts may avoid surgical replacements by employing more straightforward treatment strategies. For instance, one case highlighted a patient who had maintained a shunt for an extended period without requiring replacement. When symptoms eventually prompted a need for intervention, a novel nonsurgical approach was successfully implemented, yielding durable results without the necessity for revision surgery. This particular case underscores the potential benefits of alternative treatment options for hydrocephalus patients, particularly for those at high risk of complications from traditional surgical methods (3,4).
In light of these considerations, there is a growing need for alternative treatment modalities that can minimize the need for invasive procedures. One promising avenue is the theoretical basis for tactile stimulation of the shunt pump. This non-invasive approach aims to dislodge minor obstructions or enhance CSF flow through mechanical manipulation of the shunt. Although the exact mechanism remains unclear, it is hypothesized that regular massage of the shunt pump may help maintain its patency and functionality, particularly in cases involving partial obstruction or calcification (5,6).
This case report explores the application of the tactile stimulation method in a patient with a long-standing VP shunt, providing preliminary evidence of its viability as an alternative to surgical revision. By highlighting this non-invasive strategy, we hope to encourage further investigation into less invasive treatments that could significantly improve the quality of life for hydrocephalus patients.
Case
A 40-year-old female patient arrived at the emergency department of Abulfazl Hospital in Kashmar City, Iran, presenting with a variety of concerning symptoms, including severe headaches, hypertension, blurred vision, weakness, lethargy, nausea, and photophobia. Despite receiving supportive treatment and undergoing a thorough clinical examination, her symptoms did not improve, which prompted the attending physician to order both a brain CT scan and an MRI (Figure 1).
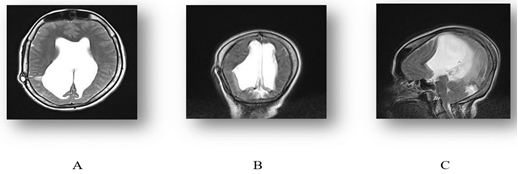
Figure 1. Brain MRI images showing the Hydrocephalus and VP shunt reservoir. (A) T2 axial view demonstrating Hydrocephalus and shunt reservoir. (B) T2 coronal view highlighting the shunt's position and enlarged lateral ventricles. (C) T2 sagittal view showing the ventricular enlargement.
The imaging results revealed the presence of hydrocephalus and a cerebral shunt, although neither the patient nor her companion were aware that a shunt surgery had been performed over 40 years prior. A consultation with a neurologist led to further examination and imaging, confirming that the shunt tube had calcified over the years and had shortened due to the patient's physical growth since its placement in infancy.
Following these findings, the patient was referred to Mashhad City in Iran and admitted to Ghaem Hospital for further evaluation and potential shunt replacement surgery. During this process, the patient's companions managed to contact the original surgeon who performed the shunt placement when the patient was just one year old. After a comprehensive clinical examination and review of the patient's paraclinical findings, the surgeon concluded that the shunt pump was still functioning properly after four decades, thus negating the need for replacement.
Instead, the patient was advised to implement a tactile regimen, which involved performing 15 massages per day on the subcutaneously installed VP shunt pump. Each massage session lasted approximately 2 min, during which gentle pressure was applied to facilitate CSF flow. The technique involved making circular motions around the pump area to ensure even pressure distribution. This regimen was maintained over a period of 10 days.
Following the completion of the tactile regimen, the patient returned for a six-month follow-up that included both clinical evaluation and brain imaging. The results were remarkably positive, indicating a complete resolution of symptoms and no evidence of shunt dysfunction or any complications.
Discussion
Hydrocephalus is a neurological disorder characterized by the abnormal accumulation of CSF in the brain's ventricles, which can lead to increased intracranial pressure and damage to brain tissue. This condition can affect individuals at any age but is most frequently observed in infants and older adults. Hydrocephalus may present as a congenital anomaly in infants or as a complication arising from premature birth. In adults, it can result from various medical issues, including infections, head injuries, or tumor development. Symptoms of hydrocephalus can differ based on the patient’s age and the severity of the condition. In infants, symptoms may include macrocephaly (an unusually large head), vomiting, irritability, and seizures. Conversely, adults may experience headaches, nausea, vision disturbances, difficulties with balance and coordination, and cognitive impairments (1, 5).
Treatment for hydrocephalus typically involves surgical intervention to either remove the excess CSF or divert it away from the brain, thereby relieving intracranial pressure. Shunt procedures remain the most prevalent surgical option, though they come with potential complications like infection, malfunction, and blockage. Alternative treatment methods, such as endoscopic third ventriculostomy (ETV) and choroid plexus cauterization (CPC), are currently being explored as possible substitutes for traditional shunt procedures (3,4). A cross-sectional survey was conducted to evaluate the impact of shunt devices on patients' lives. The results revealed that 81% of patients required at least one shunt revision surgery, with an average of 10 revision surgeries per patient (ranging from 1 to 200 surgeries). The primary reasons for shunt revision included obstruction (60%), shunt migration (47%), and infection (35%) (7). These findings underscore the significant challenges that shunt treatment poses for hydrocephalus patients, highlighting the urgent need for alternative treatments with improved safety and efficacy profiles.
This case illustrates the difficulties in managing hydrocephalus for patients who may face barriers to accessing adequate medical care or struggle to communicate effectively about their medical history. In order to achieve optimal outcomes for individuals with hydrocephalus, it is essential to ensure accurate diagnosis, timely treatment, and regular monitoring to preempt potential complications (1,2).
Regular follow-up and monitoring are vital components of care for patients with hydrocephalus who have undergone shunt placement. These practices facilitate the early detection of shunt-related complications and enable prompt interventions, thereby optimizing patient outcomes and reducing the risk of long-term neurological issues. Early identification of shunt malfunctions or complications is crucial to prevent further brain damage and avoid serious repercussions. Furthermore, it is important for patients and their caregivers to be educated about the signs and symptoms of shunt malfunction or infection to ensure quick diagnosis and treatment. The significance of accurate and thorough documentation of medical procedures and patient history cannot be overstated. This diligence is essential for providing optimal care for individuals with hydrocephalus, particularly for those lacking regular access to medical services or who may be unaware of their medical history. Additionally, the potential benefits of seeking consultations from multiple medical experts should be considered, as this can provide valuable insights and contribute to more effective treatment strategies (6-8).
The efficacy of non-surgical approaches highlights the potential advantages of alternative treatment options for hydrocephalus patients, particularly in scenarios where traditional surgical methods may pose considerable risks or complications. Nevertheless, before these approaches can be adopted extensively, their safety and effectiveness need to be rigorously assessed through further clinical studies. Notably, one innovative therapeutic modality involving regular tactile stimulation of the VP shunt pump proved to be remarkably effective in alleviating the patient's symptoms, aligned with findings from previous studies (5,6).
This technique eliminated the need for more invasive procedures, such as shunt replacement surgery, which often come with significant risks and potential complications. The success of this intervention underscores the potential value of non-invasive, non-pharmacological treatments in managing certain medical conditions. Continued research in this domain may provide additional insights into the effectiveness of tactile stimulation in promoting healing and symptom relief.
Conclusions
The non-surgical approach of massaging the VP shunt pump led to significant improvements in the patient's outcomes, with no shunt-related complications observed during the six-month follow-up period.
This alternative treatment method showcases the potential benefits of non-invasive interventions for hydrocephalus patients, especially in instances where traditional surgical procedures may pose substantial risks or complications. Nevertheless, further research is essential to thoroughly assess the safety and efficacy of this approach before it can be widely accepted as a treatment option.
These findings highlight the importance of personalized, multidisciplinary care for hydrocephalus patients, along with ongoing monitoring and follow-up to ensure optimal outcomes and prevent potential complications. Similarly, the use of tactile stimulation as a non-invasive intervention for VP shunt dysfunction resulted in marked improvements in the patient's symptoms, with no complications during the six-month follow-up period.
This case underscores the potential advantages of non-invasive strategies in managing shunt-related complications, particularly when surgical revision poses significant risks.
However, these findings are limited to a single case, and additional research is needed to establish the safety and effectiveness of this method. These results reinforce the necessity of personalized, multidisciplinary care for hydrocephalus patients, with continued monitoring and follow-up to ensure optimal results.
Conflict of Interest
There is no conflict of interest to be declared.
Following these findings, the patient was referred to Mashhad City in Iran and admitted to Ghaem Hospital for further evaluation and potential shunt replacement surgery. During this process, the patient's companions managed to contact the original surgeon who performed the shunt placement when the patient was just one year old. After a comprehensive clinical examination and review of the patient's paraclinical findings, the surgeon concluded that the shunt pump was still functioning properly after four decades, thus negating the need for replacement.
Instead, the patient was advised to implement a tactile regimen, which involved performing 15 massages per day on the subcutaneously installed VP shunt pump. Each massage session lasted approximately 2 min, during which gentle pressure was applied to facilitate CSF flow. The technique involved making circular motions around the pump area to ensure even pressure distribution. This regimen was maintained over a period of 10 days.
Following the completion of the tactile regimen, the patient returned for a six-month follow-up that included both clinical evaluation and brain imaging. The results were remarkably positive, indicating a complete resolution of symptoms and no evidence of shunt dysfunction or any complications.
Discussion
Hydrocephalus is a neurological disorder characterized by the abnormal accumulation of CSF in the brain's ventricles, which can lead to increased intracranial pressure and damage to brain tissue. This condition can affect individuals at any age but is most frequently observed in infants and older adults. Hydrocephalus may present as a congenital anomaly in infants or as a complication arising from premature birth. In adults, it can result from various medical issues, including infections, head injuries, or tumor development. Symptoms of hydrocephalus can differ based on the patient’s age and the severity of the condition. In infants, symptoms may include macrocephaly (an unusually large head), vomiting, irritability, and seizures. Conversely, adults may experience headaches, nausea, vision disturbances, difficulties with balance and coordination, and cognitive impairments (1, 5).
Treatment for hydrocephalus typically involves surgical intervention to either remove the excess CSF or divert it away from the brain, thereby relieving intracranial pressure. Shunt procedures remain the most prevalent surgical option, though they come with potential complications like infection, malfunction, and blockage. Alternative treatment methods, such as endoscopic third ventriculostomy (ETV) and choroid plexus cauterization (CPC), are currently being explored as possible substitutes for traditional shunt procedures (3,4). A cross-sectional survey was conducted to evaluate the impact of shunt devices on patients' lives. The results revealed that 81% of patients required at least one shunt revision surgery, with an average of 10 revision surgeries per patient (ranging from 1 to 200 surgeries). The primary reasons for shunt revision included obstruction (60%), shunt migration (47%), and infection (35%) (7). These findings underscore the significant challenges that shunt treatment poses for hydrocephalus patients, highlighting the urgent need for alternative treatments with improved safety and efficacy profiles.
This case illustrates the difficulties in managing hydrocephalus for patients who may face barriers to accessing adequate medical care or struggle to communicate effectively about their medical history. In order to achieve optimal outcomes for individuals with hydrocephalus, it is essential to ensure accurate diagnosis, timely treatment, and regular monitoring to preempt potential complications (1,2).
Regular follow-up and monitoring are vital components of care for patients with hydrocephalus who have undergone shunt placement. These practices facilitate the early detection of shunt-related complications and enable prompt interventions, thereby optimizing patient outcomes and reducing the risk of long-term neurological issues. Early identification of shunt malfunctions or complications is crucial to prevent further brain damage and avoid serious repercussions. Furthermore, it is important for patients and their caregivers to be educated about the signs and symptoms of shunt malfunction or infection to ensure quick diagnosis and treatment. The significance of accurate and thorough documentation of medical procedures and patient history cannot be overstated. This diligence is essential for providing optimal care for individuals with hydrocephalus, particularly for those lacking regular access to medical services or who may be unaware of their medical history. Additionally, the potential benefits of seeking consultations from multiple medical experts should be considered, as this can provide valuable insights and contribute to more effective treatment strategies (6-8).
The efficacy of non-surgical approaches highlights the potential advantages of alternative treatment options for hydrocephalus patients, particularly in scenarios where traditional surgical methods may pose considerable risks or complications. Nevertheless, before these approaches can be adopted extensively, their safety and effectiveness need to be rigorously assessed through further clinical studies. Notably, one innovative therapeutic modality involving regular tactile stimulation of the VP shunt pump proved to be remarkably effective in alleviating the patient's symptoms, aligned with findings from previous studies (5,6).
This technique eliminated the need for more invasive procedures, such as shunt replacement surgery, which often come with significant risks and potential complications. The success of this intervention underscores the potential value of non-invasive, non-pharmacological treatments in managing certain medical conditions. Continued research in this domain may provide additional insights into the effectiveness of tactile stimulation in promoting healing and symptom relief.
Conclusions
The non-surgical approach of massaging the VP shunt pump led to significant improvements in the patient's outcomes, with no shunt-related complications observed during the six-month follow-up period.
This alternative treatment method showcases the potential benefits of non-invasive interventions for hydrocephalus patients, especially in instances where traditional surgical procedures may pose substantial risks or complications. Nevertheless, further research is essential to thoroughly assess the safety and efficacy of this approach before it can be widely accepted as a treatment option.
These findings highlight the importance of personalized, multidisciplinary care for hydrocephalus patients, along with ongoing monitoring and follow-up to ensure optimal outcomes and prevent potential complications. Similarly, the use of tactile stimulation as a non-invasive intervention for VP shunt dysfunction resulted in marked improvements in the patient's symptoms, with no complications during the six-month follow-up period.
This case underscores the potential advantages of non-invasive strategies in managing shunt-related complications, particularly when surgical revision poses significant risks.
However, these findings are limited to a single case, and additional research is needed to establish the safety and effectiveness of this method. These results reinforce the necessity of personalized, multidisciplinary care for hydrocephalus patients, with continued monitoring and follow-up to ensure optimal results.
Conflict of Interest
There is no conflict of interest to be declared.
Type of Study: Case Report |
Subject:
Neurosurgery
Received: 2024/12/28 | Accepted: 2025/03/15 | ePublished ahead of print: 2025/04/12 | Published: 2025/04/22
Received: 2024/12/28 | Accepted: 2025/03/15 | ePublished ahead of print: 2025/04/12 | Published: 2025/04/22
References
1. Reddy GK, Bollam P, Caldito G. Long-term outcomes of ventriculoperitoneal shunt surgery in patients with hydrocephalus. World Neurosurg. 2014;81(2):404-410. [DOI:10.1016/j.wneu.2013.01.096]
2. Stone JJ, Walker CT, Jacobson M, Phillips V, Silberstein HJ. Revision rate of pediatric ventriculoperitoneal shunts after 15 years. J Neurosurg Pediatr. 2013;11(1):15-19 [DOI:10.3171/2012.9.PEDS1298]
3. Kumar V, Bodeliwala S, Singh D. Controversy about the management of hydrocephalus-shunt vs. endoscopic third ventriculostomy. Indian J Pediatr. 2017;84(8):624-628. [DOI:10.1007/s12098-017-2338-9]
4. Kulkarni AV, Drake JM, Mallucci CL, Sgouros S, Roth J, Constantini S. Endoscopic third ventriculostomy in the treatment of childhood hydrocephalus. J Pediatrics. 2009;155(2):254-259. [DOI:10.1016/j.jpeds.2009.02.048]
5. Karimy JK, Reeves BC, Damisah E, Duy PQ, Antwi P, David W, et al. Inflammation in acquired hydrocephalus: pathogenic mechanisms and therapeutic targets. Nat Rev Neurol. 2020;16(5): 285-296. [DOI:10.1038/s41582-020-0321-y]
6. Drake JM, Kestle JR, Tuli S. CSF shunts 50 years on-past, present and future. Child's Nerv Syst. 2000;16(10-11):800-804. [DOI:10.1007/s003810000351]
7. Mitchell KS, Zelko I, Shay T, Horen S, Williams A, Luciano M, et al. The impact of hydrocephalus shunt devices on quality of life. J Craniofac Surg. 2021;32(5): p. 1746-1750. [DOI:10.1097/SCS.0000000000007579]
8. Riva-Cambrin, J., Kestle, J.R., Holubkov, R., et al. Risk factors for shunt failure in pediatric hydrocephalus: A multicenter prospective cohort study. J Neurosurg Pediatr. 2016;17(4):382-390. [DOI:10.3171/2015.6.PEDS14670]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |