Volume 13, Issue 1 (2-2025)
J Surg Trauma 2025, 13(1): 39-41 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Jalali A, Mahdavi M, Ansari Aval Z. Report of a Rare Case of Concurrent Pneumothorax and Hemothorax in a 5-Year-old Child with Cardiac Arrest after Induction of Anesthesia. J Surg Trauma 2025; 13 (1) :39-41
URL: http://jsurgery.bums.ac.ir/article-1-465-en.html
URL: http://jsurgery.bums.ac.ir/article-1-465-en.html
Rajaie Cardiovascular Medical and Research Institute, Iran University of Medical Science, Tehran, Iran
Full-Text [PDF 359 kb]
(685 Downloads)
| Abstract (HTML) (2051 Views)
Full-Text: (404 Views)
Abstract
The insertion of a central venous catheter (CVC) is a necessary procedure prior to pediatric cardiac surgery. Although CVC insertion is generally safe, the occurrence of complications, while infrequent, can include the rare combination of pneumothorax and hemothorax. This study reports a rare case of concurrent pneumothorax and hemothorax in a 5-year-old child with cardiac arrest after induction of anesthesia. A 5-year-old patient, eligible for either the Fontan procedure, suffered a cardiac arrest following CVC insertion. An echocardiogram, performed immediately, ruled out cardiac tamponade. However, the presence of both hemothorax and pneumothorax necessitated the insertion of a pigtail catheter and chest tube. In pediatric patients requiring CVC via the subclavian vein, it is prudent to establish peripheral venous access a priori. This precautionary measure ensures the availability of a conduit for fluid resuscitation, should the need arise.
Key words: Central Venous Catheter (CVC), Heart Arrest, Hemothorax, Pneumothorax
Introduction
The insertion of a central venous catheter (CVC), initially documented in 1952, is a prevalent procedure employed in both operating rooms and intensive care unit (ICU) settings. Its applications include monitoring central venous pressure, establishing reliable intravenous access for medication delivery, hemodynamic assessment, nutritional support, administration of large-volume transfusions, and facilitating dialysis when peripheral venous access is inadequate or contraindicated (1-4). The CVC offers a valuable approach, especially for individuals undergoing extensive surgical procedures or those in critically ill conditions necessitating close monitoring and the administration of potent inotropic and vasopressor medications. Nevertheless, the insertion of a CVC carries the potential for several adverse events, including arterial puncture, hematoma formation, pneumothorax, hemothorax, catheter-related infections, and thrombotic complications. The CVCs are typically inserted into the subclavian, internal jugular, or femoral veins. However, access to the subclavian vein is associated with a high occurrence of pneumothorax, while femoral vein puncture carries a high risk of infection (5). The present study reports a rare case of concurrent pneumothorax and hemothorax in a 5-year-old child with cardiac arrest after induction of anesthesia.
Case
A 5-year-old child with a history of the Glenn procedure was presented for evaluation for the Fontan procedure. Echocardiography revealed a Glenn shunt, single ventricle physiology, and cyanosis. Following the induction of anesthesia and unsuccessful attempts to establish central venous access via the right and left internal jugular and subclavian veins, the patient developed hypotension, bradycardia, and subsequently, asystole. Cardiopulmonary resuscitation (CPR) was administered to the patient for approximately 25 min.
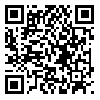
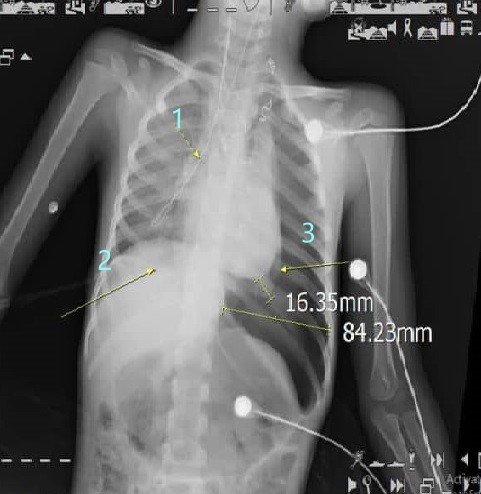
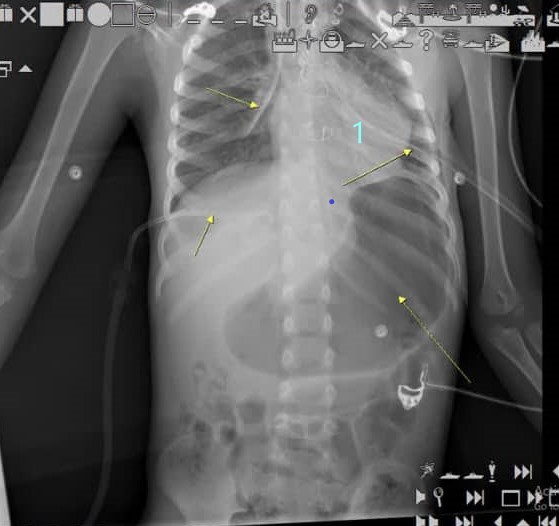
The patient’s blood pressure was successfully restored. Subsequently, an echocardiogram, including views of the pericardial and pleural spaces, was carried out. A pigtail catheter was inserted into the right pleural space, resulting in the drainage of approximately 500 cc of dark blood. A portable chest X-ray was then obtained, which revealed a left-sided tension pneumothorax. A size 16 French chest tube was inserted into the left pleural space, resulting in the drainage of approximately 100 mL of blood and air (Figures 1-3). One unit of packed red blood cells was transfused (approximately six ampules of epinephrine were injected during CPR). Due to the cessation of further drainage and the maintenance of acceptable blood pressure, the patient was transferred to the ICU for treatment of metabolic acidosis and anemia. On the same day, the patient was extubated and subsequently underwent the Fontan procedure 10 days post-operatively.
The insertion of a central venous catheter (CVC) is a necessary procedure prior to pediatric cardiac surgery. Although CVC insertion is generally safe, the occurrence of complications, while infrequent, can include the rare combination of pneumothorax and hemothorax. This study reports a rare case of concurrent pneumothorax and hemothorax in a 5-year-old child with cardiac arrest after induction of anesthesia. A 5-year-old patient, eligible for either the Fontan procedure, suffered a cardiac arrest following CVC insertion. An echocardiogram, performed immediately, ruled out cardiac tamponade. However, the presence of both hemothorax and pneumothorax necessitated the insertion of a pigtail catheter and chest tube. In pediatric patients requiring CVC via the subclavian vein, it is prudent to establish peripheral venous access a priori. This precautionary measure ensures the availability of a conduit for fluid resuscitation, should the need arise.
Key words: Central Venous Catheter (CVC), Heart Arrest, Hemothorax, Pneumothorax
Introduction
The insertion of a central venous catheter (CVC), initially documented in 1952, is a prevalent procedure employed in both operating rooms and intensive care unit (ICU) settings. Its applications include monitoring central venous pressure, establishing reliable intravenous access for medication delivery, hemodynamic assessment, nutritional support, administration of large-volume transfusions, and facilitating dialysis when peripheral venous access is inadequate or contraindicated (1-4). The CVC offers a valuable approach, especially for individuals undergoing extensive surgical procedures or those in critically ill conditions necessitating close monitoring and the administration of potent inotropic and vasopressor medications. Nevertheless, the insertion of a CVC carries the potential for several adverse events, including arterial puncture, hematoma formation, pneumothorax, hemothorax, catheter-related infections, and thrombotic complications. The CVCs are typically inserted into the subclavian, internal jugular, or femoral veins. However, access to the subclavian vein is associated with a high occurrence of pneumothorax, while femoral vein puncture carries a high risk of infection (5). The present study reports a rare case of concurrent pneumothorax and hemothorax in a 5-year-old child with cardiac arrest after induction of anesthesia.
Case
A 5-year-old child with a history of the Glenn procedure was presented for evaluation for the Fontan procedure. Echocardiography revealed a Glenn shunt, single ventricle physiology, and cyanosis. Following the induction of anesthesia and unsuccessful attempts to establish central venous access via the right and left internal jugular and subclavian veins, the patient developed hypotension, bradycardia, and subsequently, asystole. Cardiopulmonary resuscitation (CPR) was administered to the patient for approximately 25 min.
The patient’s blood pressure was successfully restored. Subsequently, an echocardiogram, including views of the pericardial and pleural spaces, was carried out. A pigtail catheter was inserted into the right pleural space, resulting in the drainage of approximately 500 cc of dark blood. A portable chest X-ray was then obtained, which revealed a left-sided tension pneumothorax. A size 16 French chest tube was inserted into the left pleural space, resulting in the drainage of approximately 100 mL of blood and air (Figures 1-3). One unit of packed red blood cells was transfused (approximately six ampules of epinephrine were injected during CPR). Due to the cessation of further drainage and the maintenance of acceptable blood pressure, the patient was transferred to the ICU for treatment of metabolic acidosis and anemia. On the same day, the patient was extubated and subsequently underwent the Fontan procedure 10 days post-operatively.
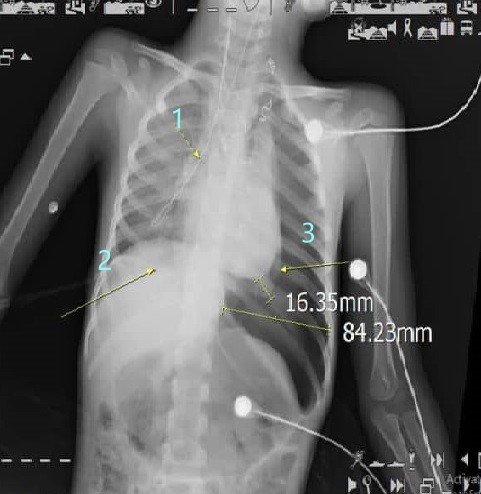
Figure 1. (1) Central venous line; (2) pigtail catheter; (3) Pneumothorax size (16.35 mm is the width of lung and 84.23 mm is the width of pneumothorax)
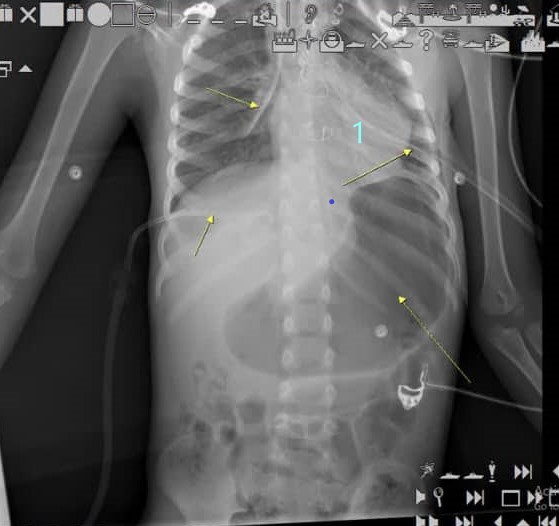
Figure 2. (1) Implantation chest tube
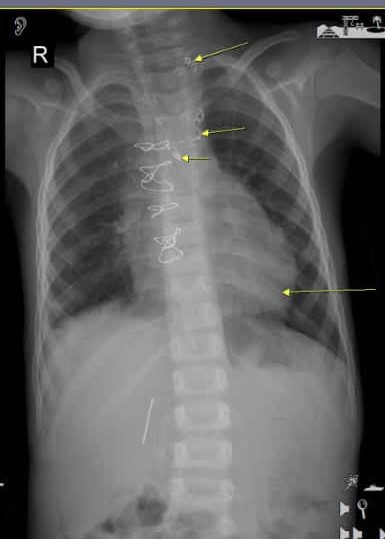
Figure 3. Position of the lung improved after performing the Fontan procedure
Discussion
Cardiac surgery, being a procedure that exposes patients to significant surgical stress, carries a high risk of postoperative complications affecting the heart, lungs, kidneys, and central nervous system. One of the procedures that, although essential during cardiac surgery and later in the intensive care unit, is the insertion of a central venous catheter; however, it also carries its own risks and complications. The CVC insertion carries several complications, including pneumothorax, hemothorax, hematoma, hydrothorax, air embolism, clotting, and infection. The incidence of its life-threatening complications is estimated to be between 0.02% and 1.5% (3,5,6). In complex surgical cases or patients with complex conditions, multiple venous accesses are often required for treatment. As a result, CVC is the preferred method. The internal jugular, subclavian, and femoral veins are frequently used as insertion sites. Subclavian vein catheterization is the preferred method because of its association with lower rates of infection and thrombotic adverse effects. However, it is more frequently linked to mechanical complications, such as pneumothorax and hemothorax. Risk factors associated with adverse effects during subclavian vein catheterization comprise female sex, underweight or overweight status, prior catheterization, history of surgery or radiotherapy in the catheter placement area, etc. In this case, given the patient’s low weight and the fact that venous access was obtained from the subclavian vein, both factors presented a risk of pneumothorax and hemothorax (5).
Ultrasound-guided CVC offers significant advantages over anatomical landmark-based approaches, demonstrably reducing both the failure rate (from 55% to 8%) and the complication rate (from 41% to 4%). Consequently, the implementation of appropriate insertion techniques, including training in ultrasound-guided methods, is strongly recommended to mitigate the risk of life-threatening complications. Regarding pneumothorax management, research suggests that a pigtail catheter is an appropriate intervention for cases exceeding 30%, a criterion met by the patient’s substantial pneumothorax (7).
Conclusions
While complications arising from CVC insertion, including concurrent hemothorax and pneumothorax, are infrequent, it is crucial to mitigate serious risks, such as cardiac arrest and hemodynamic instability. In conjunction with the utilization of ultrasound-guided techniques, it is imperative to establish a peripheral venous line prior to CVC insertion to facilitate fluid administration in the event of hemodynamic instability. Additionally, it is essential to monitor changes via pulse oximetry; a decrease in oxygen saturation should raise suspicion for pneumothorax, necessitating immediate and appropriate intervention.
Ultrasound-guided CVC offers significant advantages over anatomical landmark-based approaches, demonstrably reducing both the failure rate (from 55% to 8%) and the complication rate (from 41% to 4%). Consequently, the implementation of appropriate insertion techniques, including training in ultrasound-guided methods, is strongly recommended to mitigate the risk of life-threatening complications. Regarding pneumothorax management, research suggests that a pigtail catheter is an appropriate intervention for cases exceeding 30%, a criterion met by the patient’s substantial pneumothorax (7).
Conclusions
While complications arising from CVC insertion, including concurrent hemothorax and pneumothorax, are infrequent, it is crucial to mitigate serious risks, such as cardiac arrest and hemodynamic instability. In conjunction with the utilization of ultrasound-guided techniques, it is imperative to establish a peripheral venous line prior to CVC insertion to facilitate fluid administration in the event of hemodynamic instability. Additionally, it is essential to monitor changes via pulse oximetry; a decrease in oxygen saturation should raise suspicion for pneumothorax, necessitating immediate and appropriate intervention.
Conflict of Interest
The authors declare there is no conflict of interest.
Type of Study: Case Report |
Subject:
Heart Surgery
Received: 2025/02/14 | Accepted: 2025/03/17 | ePublished ahead of print: 2025/04/12 | Published: 2025/04/22
Received: 2025/02/14 | Accepted: 2025/03/17 | ePublished ahead of print: 2025/04/12 | Published: 2025/04/22
References
1. Park JH, Song J, Oh PW. Massive hemothorax after central venous catheter insertion in a patient with multiple trauma. J Dent Anesth Pain Med. 2021;21(1):81-85. [DOI:10.17245/jdapm.2021.21.1.81]
2. Gong TW, Zhu YH, Zhao PC, Zhang F. Massive hemothorax secondary to internal jugular vein central venous catheter placement in a patient undergoing spinal surgery complicated by chest trauma: a case report. J Cardiothoracic Surg. 2023;18(1):104. [DOI:10.1186/s13019-023-02194-5]
3. Girgin NK, Arici S, Turker G, Otlar B, Hotaman L, Kutlay O. Delayed pneumothorax and contralateral hydrothorax induced by a left subclavian central venous catheter: a case report. Clinics. 2010;65(5):562-565. [DOI:10.1590/S1807-59322010000500016]
4. Dib J, Boutari R, Yaacoub B, Al Khalil N, Al Ayoubi M, Itani O. Hemothorax occurring after central venous catheter removal: a case report. Int J Clin Res. 2023;3(1):37-41. [DOI:10.38179/ijcr.v3i1.123]
5. Bae JM. A rare case of massive hemothorax due to central venous catheterization treated with angiographic stent implantation. Korean J Crit Care Med. 2015;30(1):18-21. [DOI:10.4266/kjccm.2015.30.1.18]
6. Tsotsolis N, Tsirgogianni K, Kioumis I, Pitsiou G, Baka S, Papaiwannou A, et al. Pneumothorax as a complication of central venous catheter insertion. Ann Transl Med. 2015;3(3):40.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |