BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
URL: http://jsurgery.bums.ac.ir/article-1-177-en.html

 , Freshteh Ghaderi
, Freshteh Ghaderi 

 , Mohamadreza Akbari
, Mohamadreza Akbari 
 , Kayhan Mizani
, Kayhan Mizani 
 , Mahsa Moalemi
, Mahsa Moalemi 
 , Aliasghar Moeinipour *
, Aliasghar Moeinipour * 


Pericardial window in tamponade and sever LV systolic dysfunction after acute myocarditis
Hamid Hoseinikhah1, Freshteh Ghaderi2, Mohamadreza Akbari3, Kayhan Mizani4, Mahsa Moallemi4, Aliasghar Moeinipour5*![]()
1Assistant Professor, Department of Cardiac Surgery, Faculty of Medical Science, Mashhad University of Medical Sciences, Mashhad, Iran
2Assistant Professor of Cardiology, Fellowship of Echocardiography, Preventive Cardiovascular Care Research Center, Faculty of Medical science, Mashhad University of Medical Sciences, Mashhad, Iran
3General Physician, Faculty of Medical Science, Mashhad University of Medical Sciences, Mashhad, Iran
4Student Research Committee, Faculty of Medicine, Mashhad University of Medical Sciences, Mashhad, Mashhad, Iran
5Associated professor, Department of Cardiac Surgery, Faculty of medical science, Mashhad University of Medical Sciences, Mashhad, Iran
Received: January 27, 2019 Revised: March 02, 2019 Accepted: March 02, 2019
|
Abstract The case in this study was a 33-year-old woman suffering from acute pericardial tamponade with severe left ventricular systolic dysfunction (LVEF=10%) after myocarditis as a result of possible viral respiratory infection. The diagnosis was confirmed with two transthoracic echocardiography (TTE) evaluation showing moderate pericardial effusion with diastolic right atrium and ventricle collapse. The hemodynamic and respiratory condition of patient was unstable and emergent. The drainage of pericardial space was life-saving with good results. Key words: Cardiac surgery, Myocarditis, Pericardial tamponade |
Introduction
Pericardial tamponade is one of the most common diseases with many etiologies (1-3). Many underlying diseases can lead to the accumulation of excessive fluid in limited pericardial space resulting in an adverse effect on cardiac function, especially cardiac filling during the diastolic phase of the cardiac cycle. Different types of metastases, such as breast and lung cancer, chronic renal failure, hypothyroidism, congestive heart failure, are responsible for the majority of chronic massive pericardial effusion (4, 5). This can lead to the acute accumulation of fluid in pericardial space secondary to the infectious and inflammatory process in some cases. Many bacterial and viral infections of the upper respiratory tract can affect the myocardium layer of the heart. Moreover, fulminant myocarditis leads to the accumulation of secondary inflammatory fluid in the pericardial space, resulting in acute tamponade with tremendous effect on cardiac function (6).
Cases
The case in this study was a 33-year-old woman with no history of cardiac disease. After referral to our center (Imam Reza Hospital), she was diagnosed with acute tamponade secondary to acute myocarditis few days after upper respiratory

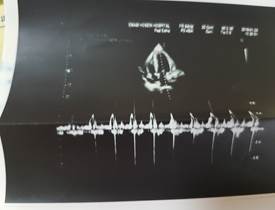

Figures 1, 2, 3: Transthoracic echocardiography examination of the patient
tract infection. The patient was in an unstable condition. Peripheral pulses were filiform and end extremities were cold. Blood pressure was 80/60 despite epinephrine support and the patient had respiratory distress with tachypnea (rr=35) and resting dyspnea and orthopnea.
In TTE evaluation, moderate pericardial effusion with a maximum diameter of fluid 1.8 cm around right ventricle and right atrium and right ventricular diastolic collapse was confirmed (figures1-3). However, the exam was indicative of severe LV systolic dysfunction (EF=10%), which was compatible with the inotropic dependency of the patient and unsatisfactory hemodynamic status. The patient was transferred to the operating room and after a comprehensive examination of central vein line, arterial line with subxyphoid approach drainage of pericardial space after pericardiotomy. In this regard, about 500 cc blood-free fluids were removed from the cavity, and the pericardial space was drained. The pericardial fluid sample was sent to the laboratory and the patients were transferred to intensive care unit after the surgery. The patient was discharged from hospital 7 days after the surgery in a good condition. In the follow-up session, her ejection fraction was increased to 35%, and the results of laboratory and pathologic examinations revealed no specific finding.
Discussion
Although most cases of pericardial tamponade are a chronic process with known etiology, the uncommonly acute accumulation of reactive fluid in pericardial space after the inflammatory and infectious process of myocardium layer of the heart can lead to acute tamponade (7). Compared to chronic tamponade, acute tamponade can be symptomatic with a lower amount of fluid (may be less than 100 ccs). In many cases of acute tamponade after myocarditis, a history of viral upper respiratory tract infection was noted (8). Influenza myocarditis is presented by a viral infectious process that decreases with cardiac function. Spontaneous recovery of myocardium function is the most common result that can be expected, although there have been rare case reports of no regression of cardiac failure,
and finally progression to a chronic, dilated cardiomyopathy, and congestive heart failure (9, 10). Acute myocarditis can cause severe left ventricular systolic dysfunction. In many cases, left ventricular systolic dysfunction is progressively reduced, and the elimination of the inflammatory process is generally followed by gradual resumption of the left ventricular systolic function to the normal range (11, 12).
Conclusions
Acute myocarditis with pericardial tamponade although can be lethal but with proper and Timely Surgical Intervention have a good prognosis.
Conflict of Interest
Authors declared no conflicts of interest.
References
1. Paddock CD, Liu L, Denison AM, Bartlett JH, Holman RC, Deleon-Carnes M, et al. Myocardial injury and bacterial pneumonia contribute to the pathogenesis of fatal influenza B virus infection. J Infect Dis.
2012; 205(6):895-905. PMID: 22291193 DOI: 10.1093/infdis/jir861
2. Taremi M, Amoroso A, Nace HL, Gilliam BL. Influenza B-induced refractory cardiogenic shock: a case report. BMC Infect Dis. 2013; 13(1):452. PMID: 24079537 DOI: 10.1186/1471-2334-13-452
3. Frank H, Wittekind C, Liebert UG, Siekmeyer M, Siekmeyer W, Schuster V, et al. Lethal influenza B myocarditis in a child and review of the literature for pediatric age groups. Infection. 2010; 38(3):231-5. PMID: 20358246 DOI: 10.1007/s15010-010-0013-4
4. Kato S, Morimoto SI, Hiramitsu S, Nomura M, Ito T, Hishida H. Use of percutaneous cardiopulmonary support of patients with fulminant myocarditis and cardiogenic shock for improving prognosis. Am J Cardiol. 1999; 83(4):623-5. PMID: 10073879
5. Sagristà-Sauleda J, Mercé J, Permanyer-Miralda G, Soler-Soler J. Clinical clues to the causes of large pericardial effusions. Am J Med. 2000; 109(2):95-101. PMID: 10967149
6. Theleman KP, Kuiper JJ, Roberts WC. Acute myocarditis (predominately lymphocytic) causing sudden death without heart failure. Am J Cardiol. 2001; 88(9):1078-83. PMID: 11704019
7. Kumar K, Guirgis M, Zieroth S, Lo E, Menkis AH, Arora RC, et al. Influenza myocarditis and myositis: case presentation and review of the literature. Can J Cardiol. 2011; 27(4):514-22. PMID: 21652168 DOI: 10.1016/j.cjca.2011.03.005
8. Estabragh ZR, Mamas MA. The cardiovascular manifestations of influenza: a systematic review. Int J Cardiol. 2013; 167(6):2397-403. PMID: 23474244 DOI: 10.1016/j.ijcard.2013.01.274
9. Brown CA, O'Connell JB. Myocarditis and idiopathic dilated cardiomyopathy. Am J Med.1995; 99(3):309-14. PMID: 7653492
10. See DM, Tilles JG. Viral myocarditis. Rev Infect Dis. 1991; 13(5):951-6. PMID: 1962111
11. Aretz HT, Billingham ME, Edwards WD, Factor SM, Fallon JT, Fenoglio JJ Jr, et al. Myocarditis. A histopathologic definition and classification. Am J Cardiovasc Pathol. 1987; 1(1):3-14. PMID: 3455232
12. Mendes LA, Dec GW, Picard MH, Palacios IF, Newell J, Davidoff R. Right ventricular dysfunction: an independent predictor of adverse outcome in patients with myocarditis. Am Heart J. 1994; 128(2):301-7. PMID: 8037097
Received: 2019/01/27 | Accepted: 2019/03/2 | ePublished ahead of print: 2019/03/11 | Published: 2019/06/12
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |