Volume 13, Issue 1 (2-2025)
J Surg Trauma 2025, 13(1): 8-13 |
Back to browse issues page
Ethics code: IR.BUMS.REC.1401.302
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Babaiyan S, Omidvar L, Abdollahi H. Comparing Trapezius Muscle Compression and Chin Lift for Laryngeal Mask Insertion Timing in Non-Relaxed Anesthesia in patients undergoing orthopedic elective surgery. J Surg Trauma 2025; 13 (1) :8-13
URL: http://jsurgery.bums.ac.ir/article-1-459-en.html
URL: http://jsurgery.bums.ac.ir/article-1-459-en.html
Department of Anesthesiology, School of Medicine, Birjand University of Medical Sciences, Birjand, Iran
Full-Text [PDF 417 kb]
(218 Downloads)
| Abstract (HTML) (690 Views)
Results
In the present study, the mean age of the 138 patients, ranging from 18 to 70 years, was 37.7±13.4 years. Hemodynamic changes were compared between the two groups of patients that underwent the trapezius squeezing or chin lift maneuver to indicate the appropriate time for laryngeal mask insertion. The mean age in the trapezius squeezing and the chin lift groups were 38±13.48 and 37.4±13.37 years, respectively, which showed no significant statistical difference (P-value=0.893).
A percentage of 73.9% (N=51) of the patients in the trapezius squeezing group and 71% (N=49) of them in the chin lift group were male, which showed no significant statistical difference (P-value=0.849) (Table 1). Systolic blood pressure declined after induction and insertion of the LMA in both groups compared to the pre-induction (P-value<0.001). In both groups, 2 min after LMA insertion, systolic blood pressure was almost similar to the systolic blood pressure after inserting the LMA (P-value=0.682, 0.911). No difference was observed for this variable between the two groups (P-value=0.269). Diastolic blood pressure declined in both groups after LMA insertion compared to the pre-induction (P-value<0.001). No significant difference was observed for this variable between the two groups (P-value=0.279) (Table 2). No significant change in arterial blood oxygenation was seen before induction, after LMA insertion, and 2 min after induction. In the present study, the heart rate after LMA insertion and 2 min after LMA insertion decreased compared to the heart rate before induction (P-value<0.001, P-value=0.050). The appropriate time for LMA insertion was slightly longer in the chin lift group; however, this difference was not statistically significant (P-value=0.114) (Table 3).
Discussion
The LMA insertion without using muscle relaxants requires sufficient anesthetic depth to suppress the undesired reflexes of the airway. In most cases, students and mentors try to insert the LMA after seeing that the muscles are relaxed, the verbal contact is broken, and the blink reflex is lost. These methods are followed by a high prevalence of adverse effects, such as cough, straining, laryngeal spasm, and consequently, the probability of failure in inserting the laryngeal mask (12). Therefore, we decided to assess the conditions of the appropriate time to insert the laryngeal mask using two maneuvers, including trapezius muscle squeezing and chin lift.
Regarding the patients’ gender, 73.9% of the patients in the trapezius squeezing group and 71% in the chin lift group were male, which showed no significant statistical difference (P=0.849).
Four patients out of 69 (5.8%) in the trapezius squeezing group and two patients in the chin lift group (2.9%) were recorded to have an unsuccessful first attempt. The lower rate of first-attempt failure in the chin lift group may be attributed to the higher intensity of stimulation and deeper anesthesia associated with this maneuver, which led to a longer time to LMA insertion and a lesser rate of gag reflex stimulation and SpO2 decline.
Kouzegaran et al. studied orthopedic patients using propofol for induction and indicated that the success rate of the first attempt to insert LMA was higher in the chin lift group; however, there was no significant difference between the two groups (14). Liu et al. studied patients of 6 months to 3 years of age undergoing minor surgeries and anesthesia induction with 6% sevoflurane. They suggested that the trapezius squeezing test demonstrates greater effectiveness in assessing the suitability for LMA insertion in infants and young children under sevoflurane anesthesia compared to the jaw thrust maneuver (15). Hooda et al. studied patients by only employing the trapezius squeezing maneuver and reported a first-attempt success of 96% (16). Chang et al. studied patients undergoing minor surgeries and anesthesia induction with 6% sevoflurane and reported a significantly higher success rate of LMA insertion in the trapezius squeezing group in comparison with the chin lift group, which is contrary to the results of the present work (13). Concerning the results of these studies, it seems that the anesthetic drug used for induction can impact the patient's response to these maneuvers. However, we used sodium thiopental for anesthesia induction, which decreases the incidence of cough, gag reflex, and airway stimulation as well as propofol which increases the success rate of LMA insertion.
Appropriate times for laryngeal mask insertion in the trapezius squeezing group and the chin lift group were 90.14 and 93.62 seconds, respectively, which can be due to the higher severity of pain caused by the chin lift maneuver in comparison to the trapezius squeezing maneuver. This finding is discordant with the findings of Kouzegaran et al., who recorded that the mean appropriate time for laryngeal mask insertion was higher in the trapezius squeezing group than in the chin lift group (14). This difference in the response to these maneuvers in various studies can be due to the difference in the anesthetic drugs.
In both groups, the systolic blood pressure declined after LMA insertion, which, in addition to the anxiolytic effects of midazolam and the blood pressure-lowering effects of anesthetic drugs, may be attributed to the timely insertion of the LMA. This result indicates that applying these maneuvers was beneficial for determining the appropriate time for LMA insertion and prevented the sympathetic stimulation that leads to blood pressure rises, which is linked to lower cardiovascular risks in elderly patients and those with comorbidities. In both groups, the systolic blood pressure 2 min after anesthesia induction was almost similar to the level immediately after induction, likely due to the increase in anesthesia depth and the proper dosing of the used drugs. No difference was observed for this variable between the two groups, which is in concordance with Kouzegaran et al.’s study, reporting no difference in the vital signs between the two groups (14).
Zeinali et al. reported a systolic blood pressure rise in the LMA insertion group, which had no significance compared to the endotracheal intubation group (17). The discordance between this study and the present work can be caused by insufficient anesthesia depth in the case of early LMA insertion.
Liu et al. reported no significant change in the blood pressure of both groups after LMA insertion, which could be due to the suppression of sympathetic response by sevoflurane (15).
Moreover, the stability of blood pressure 2 min after induction, which is after the LMA insertion, indicates the usefulness of these maneuvers for determining the proper time for LMA insertion.
In both groups, the diastolic blood pressure declined after LMA insertion, possibly due to the LMA insertion being performed at an appropriate time. No significant difference between the groups was observed for this variable. The continuation of diastolic blood pressure decline in both groups 2 min after induction can be due to the proper dosing of anesthetic drugs and the appropriate time of LMA insertion.
Zeinali et al. reported an increase in diastolic blood pressure after LMA insertion that was not significant, which is discordant with our findings. This discrepancy may be attributed to insufficient anesthesia depth in the case of early LMA insertion or inadequate dosing of the anesthetic drug (17).
Furthermore, Liu et al. reported no significant change in blood pressure in both groups, which is in line with the present study (15).
No significant change in arterial blood oxygenation was observed before induction, at the time of induction, and 2 min after induction. In addition to the appropriate determination of the timing of LMA insertion using these maneuvers—which prevented airway complications (e.g., gag reflex, straining, laryngospasm, and SpO2 decline)—this finding may also be attributed to continuous oxygenation by mask from the patient's entrance to the operating room until LMA insertion and during the surgery.
The heart rate declined at the moment after LMA insertion and 2 min after that, which can be caused by the patient’s anxiety reduction after anesthesia induction, in addition to the proper time of LMA insertion. Zeinali et al. reported an increase in blood pressure and heart rate after LMA insertion and endotracheal intubation that continued and is probably due to insufficient anesthesia depth in the case of airway instrument placement or insufficient anesthetic dosing (17). The lack of significant differences in hemodynamic parameters between the two groups reinforces the safety and efficacy of both maneuvers. These results suggest that either maneuver can effectively determine the appropriate time for LMA insertion, reducing the risk of airway-related complications and optimizing anesthetic management.
The limitation of the present work is the small available sample size and the inclusion of only adult patients. The varied distribution of drugs in the pediatric population may lead to different results; therefore, studying the pediatric population with different drugs is recommended.
Conclusions
According to the results of this study, it is suggested that the mentors and students consider utilizing any of the mentioned maneuvers to determine the appropriate time of laryngeal mask insertion to prevent undesirable hemodynamic changes in the elderly or patients with cardiovascular comorbidities that can cause injury.
Acknowledgments
We would like to thank everyone who collaborated on this research.
Funding
The authors declare there were no funding sources for this work.
Conflict of Interest
The authors declare that there is no conflict of interest.
Full-Text: (161 Views)
Abstract
Introduction: The maintenance of an adequate airway during surgery is essential for effective oxygenation and ventilation in anesthetized patients. The optimal timing for laryngeal mask airway (LMA) insertion to prevent airway complications and enhance patient safety remains uncertain. The present study aimed to compare trapezius muscle compression and chin lift maneuvers as indicators of appropriate LMA insertion timing.
Methods: This randomized controlled trial (RCT) included 138 patients undergoing elective orthopedic surgery at Imam Reza Hospital, Birjand University of Medical Sciences, Iran. Patients were randomly assigned using block randomization with stratification into two groups: trapezius muscle squeezing or chin lift maneuvers. Anesthesia induction was performed with midazolam, fentanyl, and sodium thiopental. The assigned maneuver was applied at 20-second intervals until no motor response was observed; the LMA was inserted at this point. Unsuccessful attempts were defined by complications, such as laryngospasm, bronchospasm, or oxygen desaturation (<90%). Hemodynamic parameters, LMA insertion time, and success rates were recorded and compared between the groups.
Results: Systolic blood pressure in mmHg declined after insertion of the LMA in both groups compared to the pre-induction (P-value<0.001). In addition, diastolic blood pressure in mmHg showed a significant reduction in both groups after LMA insertion compared to the pre-induction (P-value<0.001). In the present study, the heart rate (beats per minute [bpm]) decreased significantly after LMA insertion and 2 min post-insertion compared to the pre-induction (P-value<0.001, P-value=0.050). The success rate for LMA insertion was high in both groups, with 94.2% (N=65) in the trapezius squeezing group and 97.1% (N=67) in the chin lift group. The time to successful LMA insertion was slightly longer in the chin lift group (93.62±13.50 seconds) compared to the trapezius squeezing group (90.14±12.18 seconds); however, this difference was not statistically significant (P-value=0.114).
Conclusion: The time for LMA insertion was slightly longer in the chin lift group, but this difference was not statistically significant. Both maneuvers showed equally high success rates for LMA insertion. Hemodynamic changes, including blood pressure and heart rate, declined similarly in both groups, with no significant differences. Therefore, both the trapezius squeezing and chin lift maneuvers are equally effective for successful LMA insertion.
Key words: Anesthesia, Elective Surgical Procedures, Hemodynamic Monitoring, Laryngeal Mask Airway
Introduction
For a patient undergoing surgery, a patent and proper airway are the primary elements to maintain efficient breathing. Some instruments provide proper oxygenation and ventilation for the anesthetized patient during surgery. Endotracheal intubation is the most reliable way to provide an airway, which is indicated in some cases (e.g., a full stomach patient undergoing general anesthesia) (1). Laryngoscopy and endotracheal intubation can cause tachycardia, a rise in blood pressure, arrhythmia, myocardial ischemia, and an increase in intracranial pressure (2, 3). A laryngeal mask is a noninvasive, appropriate alternative to endotracheal intubation in short-duration surgeries, and it does not carry the risks and complications of laryngoscopy. This mask is conventionally used to obtain a safe airway and maintain spontaneous ventilation in short-duration outpatient surgeries with a patient undergoing general anesthesia (4, 5). Sufficient anesthetic depth is crucial for the insertion of this instrument since muscle relaxants are not used for this purpose. Insufficient anesthetic depth can lead to airway complications, such as bronchospasm, laryngospasm, and severe hemodynamic changes like tachycardia and hypertension (6, 7). Various techniques have been used for assessing the anesthetic depth for inserting the laryngeal mask, including the intravenous anesthetic dose, loss of verbal response, loss of the blink reflex, and relaxation of the mandible (8). Loss of verbal response and blink reflex are not appropriate indicators for the sufficiency of anesthetic depth needed for laryngeal mask insertion (7). Assessing the intravenous anesthetic dose is a complicated method not accessible in every setting (9). Loss of motor response to chin lift maneuver or trapezius squeezing has been effective for assessing the sufficient anesthetic depth for laryngeal mask insertion in adults and pediatric patients (10). Some prior studies have compared these maneuvers in patients undergoing anesthesia with inhalation anesthetics, and their results are different with variable doses of inhalation anesthetics (11). In most cases, students and mentors try to insert the laryngeal mask airway (LMA) after observing that the muscles are relaxed, the verbal contact is broken, and the blink reflex is lost. These methods are followed by a high prevalence of adverse effects, such as cough, straining, laryngeal spasm, and consequently, the probability of failure in inserting the laryngeal mask (12). Therefore, we decided to assess the conditions of the appropriate time to insert the laryngeal mask by using the two maneuvers of trapezius muscle squeezing and chin lift. The present study aimed to identify the most reliable maneuver to predict appropriate anesthetic depth for LMA insertion in patients undergoing general anesthesia with sodium thiopental. By examining these maneuvers, the purpose was to provide clearer guidance for clinicians to minimize the risk of complications during LMA insertion and optimize patient safety.
Methods
The present study is a clinical trial with patients undergoing orthopedic elective surgery and general anesthesia at Imam Reza Hospital of Birjand University of Medical Sciences, Iran. The Ethical code was obtained (IR.BUMS.REC.1401.302), and the trial was registered in the Iranian Registry of Clinical Trials with the code IRCT20221115056503N1. Notably, the study was conducted in 2022, and the Helsinki principles were implemented. First, the purpose of the study and its process were explained to the patients, and their informed consent was obtained. Their demographic information, including age and gender, was recorded in the relevant checklist. Then, the patients were randomly assigned using block randomization with stratification into two groups: trapezius muscle squeezing or chin lift maneuvers. Non-probability convenience sampling was employed for sampling. According to Chang et al., the power was set at 80%, and a P-value of less than 0.05 was considered significant for each group (69 patients per group) (13).
The inclusion criteria were patients aged between 18 and 70 who were scheduled for elective orthopedic surgery. All participants were required to have an ASA classification of I or II, reflecting a general health status without significant underlying conditions or only mild, well-managed diseases. Only patients who provided written informed consent were included in the study.
Exclusion criteria were emergency patients, uncontrolled systemic disease, hemodynamic instability, pregnancy, hypertension, drug abuse, BMI>30, neck-related movement disorders, difficulty in opening the mouth, and ventilation failure after laryngeal mask insertion.
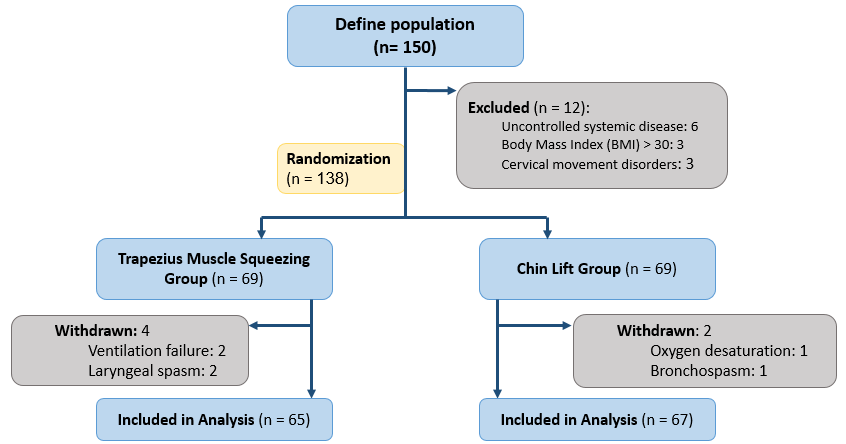
The consort flowchart (Figure 1) illustrates the participant enrollment process, inclusion and exclusion criteria, and randomization in this study.
For both groups, 0.02 mg/kg of midazolam and 2 µg/kg of fentanyl were used for anesthesia induction, and then 5 mg/kg of sodium thiopental was employed as the anesthetic. No nerve-blocking drug was used. According to the patient group, one of the chin lift or trapezius muscle squeezing maneuvers was applied at 20-second intervals from 1 min after anesthesia induction until the motor response was lost.
The appropriate time for laryngeal mask insertion was recorded as the time from the anesthesia induction to the time of losing the motor response. At that moment, a classic LMA with a suitable size based on the patient’s weight was inserted by an anesthesiologist who was not a research team member and was not informed about the study's aims. If the patient had a cough, gag, apnea, SpO2 decline to below 90%, or unusual movements within 1 min after insertion, the attempt was recorded as failed. Efficient ventilation was assessed by inspecting chest movement, performing breathing auscultation, and using capnography. Systolic and diastolic blood pressure, heart rate, and arterial blood oxygenation (SpO2) were recorded before and after LMA insertion and again 2 min after LMA insertion.
The data were analyzed using the SPSS (version 16) software. The normality of the data was assessed using the Kolmogorov-Smirnov test and the P-PLOT chart. Descriptive statistics, independent t-tests, and paired t-tests were used for data analysis at a significance level of 0.05. To adjust for baseline variables, analysis of covariance (ANCOVA) or repeated measures analysis of variance (ANOVA) was utilized as appropriate.
Introduction: The maintenance of an adequate airway during surgery is essential for effective oxygenation and ventilation in anesthetized patients. The optimal timing for laryngeal mask airway (LMA) insertion to prevent airway complications and enhance patient safety remains uncertain. The present study aimed to compare trapezius muscle compression and chin lift maneuvers as indicators of appropriate LMA insertion timing.
Methods: This randomized controlled trial (RCT) included 138 patients undergoing elective orthopedic surgery at Imam Reza Hospital, Birjand University of Medical Sciences, Iran. Patients were randomly assigned using block randomization with stratification into two groups: trapezius muscle squeezing or chin lift maneuvers. Anesthesia induction was performed with midazolam, fentanyl, and sodium thiopental. The assigned maneuver was applied at 20-second intervals until no motor response was observed; the LMA was inserted at this point. Unsuccessful attempts were defined by complications, such as laryngospasm, bronchospasm, or oxygen desaturation (<90%). Hemodynamic parameters, LMA insertion time, and success rates were recorded and compared between the groups.
Results: Systolic blood pressure in mmHg declined after insertion of the LMA in both groups compared to the pre-induction (P-value<0.001). In addition, diastolic blood pressure in mmHg showed a significant reduction in both groups after LMA insertion compared to the pre-induction (P-value<0.001). In the present study, the heart rate (beats per minute [bpm]) decreased significantly after LMA insertion and 2 min post-insertion compared to the pre-induction (P-value<0.001, P-value=0.050). The success rate for LMA insertion was high in both groups, with 94.2% (N=65) in the trapezius squeezing group and 97.1% (N=67) in the chin lift group. The time to successful LMA insertion was slightly longer in the chin lift group (93.62±13.50 seconds) compared to the trapezius squeezing group (90.14±12.18 seconds); however, this difference was not statistically significant (P-value=0.114).
Conclusion: The time for LMA insertion was slightly longer in the chin lift group, but this difference was not statistically significant. Both maneuvers showed equally high success rates for LMA insertion. Hemodynamic changes, including blood pressure and heart rate, declined similarly in both groups, with no significant differences. Therefore, both the trapezius squeezing and chin lift maneuvers are equally effective for successful LMA insertion.
Key words: Anesthesia, Elective Surgical Procedures, Hemodynamic Monitoring, Laryngeal Mask Airway
Introduction
For a patient undergoing surgery, a patent and proper airway are the primary elements to maintain efficient breathing. Some instruments provide proper oxygenation and ventilation for the anesthetized patient during surgery. Endotracheal intubation is the most reliable way to provide an airway, which is indicated in some cases (e.g., a full stomach patient undergoing general anesthesia) (1). Laryngoscopy and endotracheal intubation can cause tachycardia, a rise in blood pressure, arrhythmia, myocardial ischemia, and an increase in intracranial pressure (2, 3). A laryngeal mask is a noninvasive, appropriate alternative to endotracheal intubation in short-duration surgeries, and it does not carry the risks and complications of laryngoscopy. This mask is conventionally used to obtain a safe airway and maintain spontaneous ventilation in short-duration outpatient surgeries with a patient undergoing general anesthesia (4, 5). Sufficient anesthetic depth is crucial for the insertion of this instrument since muscle relaxants are not used for this purpose. Insufficient anesthetic depth can lead to airway complications, such as bronchospasm, laryngospasm, and severe hemodynamic changes like tachycardia and hypertension (6, 7). Various techniques have been used for assessing the anesthetic depth for inserting the laryngeal mask, including the intravenous anesthetic dose, loss of verbal response, loss of the blink reflex, and relaxation of the mandible (8). Loss of verbal response and blink reflex are not appropriate indicators for the sufficiency of anesthetic depth needed for laryngeal mask insertion (7). Assessing the intravenous anesthetic dose is a complicated method not accessible in every setting (9). Loss of motor response to chin lift maneuver or trapezius squeezing has been effective for assessing the sufficient anesthetic depth for laryngeal mask insertion in adults and pediatric patients (10). Some prior studies have compared these maneuvers in patients undergoing anesthesia with inhalation anesthetics, and their results are different with variable doses of inhalation anesthetics (11). In most cases, students and mentors try to insert the laryngeal mask airway (LMA) after observing that the muscles are relaxed, the verbal contact is broken, and the blink reflex is lost. These methods are followed by a high prevalence of adverse effects, such as cough, straining, laryngeal spasm, and consequently, the probability of failure in inserting the laryngeal mask (12). Therefore, we decided to assess the conditions of the appropriate time to insert the laryngeal mask by using the two maneuvers of trapezius muscle squeezing and chin lift. The present study aimed to identify the most reliable maneuver to predict appropriate anesthetic depth for LMA insertion in patients undergoing general anesthesia with sodium thiopental. By examining these maneuvers, the purpose was to provide clearer guidance for clinicians to minimize the risk of complications during LMA insertion and optimize patient safety.
Methods
The present study is a clinical trial with patients undergoing orthopedic elective surgery and general anesthesia at Imam Reza Hospital of Birjand University of Medical Sciences, Iran. The Ethical code was obtained (IR.BUMS.REC.1401.302), and the trial was registered in the Iranian Registry of Clinical Trials with the code IRCT20221115056503N1. Notably, the study was conducted in 2022, and the Helsinki principles were implemented. First, the purpose of the study and its process were explained to the patients, and their informed consent was obtained. Their demographic information, including age and gender, was recorded in the relevant checklist. Then, the patients were randomly assigned using block randomization with stratification into two groups: trapezius muscle squeezing or chin lift maneuvers. Non-probability convenience sampling was employed for sampling. According to Chang et al., the power was set at 80%, and a P-value of less than 0.05 was considered significant for each group (69 patients per group) (13).
The inclusion criteria were patients aged between 18 and 70 who were scheduled for elective orthopedic surgery. All participants were required to have an ASA classification of I or II, reflecting a general health status without significant underlying conditions or only mild, well-managed diseases. Only patients who provided written informed consent were included in the study.
Exclusion criteria were emergency patients, uncontrolled systemic disease, hemodynamic instability, pregnancy, hypertension, drug abuse, BMI>30, neck-related movement disorders, difficulty in opening the mouth, and ventilation failure after laryngeal mask insertion.
The consort flowchart (Figure 1) illustrates the participant enrollment process, inclusion and exclusion criteria, and randomization in this study.
For both groups, 0.02 mg/kg of midazolam and 2 µg/kg of fentanyl were used for anesthesia induction, and then 5 mg/kg of sodium thiopental was employed as the anesthetic. No nerve-blocking drug was used. According to the patient group, one of the chin lift or trapezius muscle squeezing maneuvers was applied at 20-second intervals from 1 min after anesthesia induction until the motor response was lost.
The appropriate time for laryngeal mask insertion was recorded as the time from the anesthesia induction to the time of losing the motor response. At that moment, a classic LMA with a suitable size based on the patient’s weight was inserted by an anesthesiologist who was not a research team member and was not informed about the study's aims. If the patient had a cough, gag, apnea, SpO2 decline to below 90%, or unusual movements within 1 min after insertion, the attempt was recorded as failed. Efficient ventilation was assessed by inspecting chest movement, performing breathing auscultation, and using capnography. Systolic and diastolic blood pressure, heart rate, and arterial blood oxygenation (SpO2) were recorded before and after LMA insertion and again 2 min after LMA insertion.
The data were analyzed using the SPSS (version 16) software. The normality of the data was assessed using the Kolmogorov-Smirnov test and the P-PLOT chart. Descriptive statistics, independent t-tests, and paired t-tests were used for data analysis at a significance level of 0.05. To adjust for baseline variables, analysis of covariance (ANCOVA) or repeated measures analysis of variance (ANOVA) was utilized as appropriate.
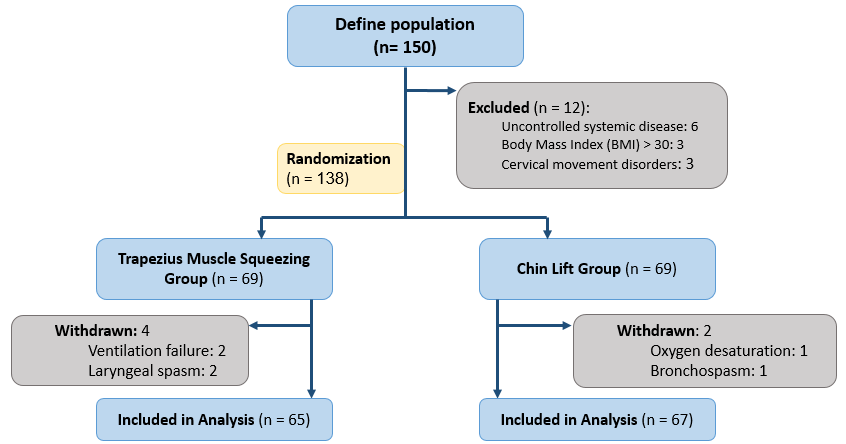
Figure 1. Flowchart of participant enrollment and allocation
Results
In the present study, the mean age of the 138 patients, ranging from 18 to 70 years, was 37.7±13.4 years. Hemodynamic changes were compared between the two groups of patients that underwent the trapezius squeezing or chin lift maneuver to indicate the appropriate time for laryngeal mask insertion. The mean age in the trapezius squeezing and the chin lift groups were 38±13.48 and 37.4±13.37 years, respectively, which showed no significant statistical difference (P-value=0.893).
A percentage of 73.9% (N=51) of the patients in the trapezius squeezing group and 71% (N=49) of them in the chin lift group were male, which showed no significant statistical difference (P-value=0.849) (Table 1). Systolic blood pressure declined after induction and insertion of the LMA in both groups compared to the pre-induction (P-value<0.001). In both groups, 2 min after LMA insertion, systolic blood pressure was almost similar to the systolic blood pressure after inserting the LMA (P-value=0.682, 0.911). No difference was observed for this variable between the two groups (P-value=0.269). Diastolic blood pressure declined in both groups after LMA insertion compared to the pre-induction (P-value<0.001). No significant difference was observed for this variable between the two groups (P-value=0.279) (Table 2). No significant change in arterial blood oxygenation was seen before induction, after LMA insertion, and 2 min after induction. In the present study, the heart rate after LMA insertion and 2 min after LMA insertion decreased compared to the heart rate before induction (P-value<0.001, P-value=0.050). The appropriate time for LMA insertion was slightly longer in the chin lift group; however, this difference was not statistically significant (P-value=0.114) (Table 3).
Table 1. Success rate of laryngeal mask insertion in studied groups
Table 2. Mean and significance of the variables before induction, after laryngeal mask insertion, and 2 min after induction in both groups
Table 3. Mean insertion time in both groups
| Intervention group | Total number of patients | Success rate of laryngeal mask insertion | Failed attempts |
| Trapezius squeezing group | 69 | 65 (94.2%) | 4 (5.8%) |
| Chin lift group | 69 | 67 (97.1%) | 2 (2.9%) |
Table 2. Mean and significance of the variables before induction, after laryngeal mask insertion, and 2 min after induction in both groups
| Variable | Study groups | Before induction | After LMA insertion | 2 min after LMA insertion | Within groups | Between groups | ||
| P1 (before and after LMA insertion) | P2 (before and 2 minutes after LMA insertion) | P3 (after LMA insertion and 2 minutes after that) | ||||||
| Systolic blood pressure | Trapezius squeezing | 126.2±15.43 | 106.86±14.27 | 106.25±14.63 | <0.001 | <0.001 | <0.001 | 0.682 |
| Chin lift | 132.91±19.33 | 109.75±14.70 | 109.33±18.70 | <0.001 | <0.001 | <0.001 | 0.911 | |
| Independent T | 0.027 | 0.269 | 0.282 | - | - | - | ||
| Diastolic blood pressure | Trapezius squeezing | 75.70±12.37 | 64.64±13.62 | 62.14±12.82 | <0.001 | <0.001 | <0.001 | 0.036 |
| Chin lift | 80.06±15.02 | 76.45±12.98 | 65.61±12.41 | <0.001 | 0.732 | 0.000 | 0.304 | |
| Independent T | 0.065 | 0.279 | 0.109 | - | - | - | ||
| Arterial blood oxygenation | Trapezius squeezing | 98.46±1.34 | 99.75±0.49 | 99.58±0.73 | <0.001 | <0.001 | <0.001 | 0.013 |
| Chin lift | 98.35±1.51 | 99.75±0.57 | 99.51±0.94 | <0.001 | <0.001 | <0.001 | 0.006 | |
| Independent T | 0.635 | 1 | 0.617 | - | - | - | ||
| Heart rate | Trapezius squeezing | 85.80±14.64 | 78.29±13.26 | 82.78±15.60 | <0.001 | <0.001 | 0.050 | 0.003 |
| Chin lift | 88.93±15.43 | 82.25±16.78 | 84.09±16.26 | <0.001 | <0.001 | 0.002 | 0.193 | |
| Independent T | 0.224 | 0.127 | 0.631 | - | - | - |
Table 3. Mean insertion time in both groups
| Variable | Groups | Mean | P-value |
| Time of laryngeal mask insertion (seconds) | Trapezius squeezing | 90.14±12.18 | 0.114 |
| Chin lift | 93.62±13.500 |
Discussion
The LMA insertion without using muscle relaxants requires sufficient anesthetic depth to suppress the undesired reflexes of the airway. In most cases, students and mentors try to insert the LMA after seeing that the muscles are relaxed, the verbal contact is broken, and the blink reflex is lost. These methods are followed by a high prevalence of adverse effects, such as cough, straining, laryngeal spasm, and consequently, the probability of failure in inserting the laryngeal mask (12). Therefore, we decided to assess the conditions of the appropriate time to insert the laryngeal mask using two maneuvers, including trapezius muscle squeezing and chin lift.
Regarding the patients’ gender, 73.9% of the patients in the trapezius squeezing group and 71% in the chin lift group were male, which showed no significant statistical difference (P=0.849).
Four patients out of 69 (5.8%) in the trapezius squeezing group and two patients in the chin lift group (2.9%) were recorded to have an unsuccessful first attempt. The lower rate of first-attempt failure in the chin lift group may be attributed to the higher intensity of stimulation and deeper anesthesia associated with this maneuver, which led to a longer time to LMA insertion and a lesser rate of gag reflex stimulation and SpO2 decline.
Kouzegaran et al. studied orthopedic patients using propofol for induction and indicated that the success rate of the first attempt to insert LMA was higher in the chin lift group; however, there was no significant difference between the two groups (14). Liu et al. studied patients of 6 months to 3 years of age undergoing minor surgeries and anesthesia induction with 6% sevoflurane. They suggested that the trapezius squeezing test demonstrates greater effectiveness in assessing the suitability for LMA insertion in infants and young children under sevoflurane anesthesia compared to the jaw thrust maneuver (15). Hooda et al. studied patients by only employing the trapezius squeezing maneuver and reported a first-attempt success of 96% (16). Chang et al. studied patients undergoing minor surgeries and anesthesia induction with 6% sevoflurane and reported a significantly higher success rate of LMA insertion in the trapezius squeezing group in comparison with the chin lift group, which is contrary to the results of the present work (13). Concerning the results of these studies, it seems that the anesthetic drug used for induction can impact the patient's response to these maneuvers. However, we used sodium thiopental for anesthesia induction, which decreases the incidence of cough, gag reflex, and airway stimulation as well as propofol which increases the success rate of LMA insertion.
Appropriate times for laryngeal mask insertion in the trapezius squeezing group and the chin lift group were 90.14 and 93.62 seconds, respectively, which can be due to the higher severity of pain caused by the chin lift maneuver in comparison to the trapezius squeezing maneuver. This finding is discordant with the findings of Kouzegaran et al., who recorded that the mean appropriate time for laryngeal mask insertion was higher in the trapezius squeezing group than in the chin lift group (14). This difference in the response to these maneuvers in various studies can be due to the difference in the anesthetic drugs.
In both groups, the systolic blood pressure declined after LMA insertion, which, in addition to the anxiolytic effects of midazolam and the blood pressure-lowering effects of anesthetic drugs, may be attributed to the timely insertion of the LMA. This result indicates that applying these maneuvers was beneficial for determining the appropriate time for LMA insertion and prevented the sympathetic stimulation that leads to blood pressure rises, which is linked to lower cardiovascular risks in elderly patients and those with comorbidities. In both groups, the systolic blood pressure 2 min after anesthesia induction was almost similar to the level immediately after induction, likely due to the increase in anesthesia depth and the proper dosing of the used drugs. No difference was observed for this variable between the two groups, which is in concordance with Kouzegaran et al.’s study, reporting no difference in the vital signs between the two groups (14).
Zeinali et al. reported a systolic blood pressure rise in the LMA insertion group, which had no significance compared to the endotracheal intubation group (17). The discordance between this study and the present work can be caused by insufficient anesthesia depth in the case of early LMA insertion.
Liu et al. reported no significant change in the blood pressure of both groups after LMA insertion, which could be due to the suppression of sympathetic response by sevoflurane (15).
Moreover, the stability of blood pressure 2 min after induction, which is after the LMA insertion, indicates the usefulness of these maneuvers for determining the proper time for LMA insertion.
In both groups, the diastolic blood pressure declined after LMA insertion, possibly due to the LMA insertion being performed at an appropriate time. No significant difference between the groups was observed for this variable. The continuation of diastolic blood pressure decline in both groups 2 min after induction can be due to the proper dosing of anesthetic drugs and the appropriate time of LMA insertion.
Zeinali et al. reported an increase in diastolic blood pressure after LMA insertion that was not significant, which is discordant with our findings. This discrepancy may be attributed to insufficient anesthesia depth in the case of early LMA insertion or inadequate dosing of the anesthetic drug (17).
Furthermore, Liu et al. reported no significant change in blood pressure in both groups, which is in line with the present study (15).
No significant change in arterial blood oxygenation was observed before induction, at the time of induction, and 2 min after induction. In addition to the appropriate determination of the timing of LMA insertion using these maneuvers—which prevented airway complications (e.g., gag reflex, straining, laryngospasm, and SpO2 decline)—this finding may also be attributed to continuous oxygenation by mask from the patient's entrance to the operating room until LMA insertion and during the surgery.
The heart rate declined at the moment after LMA insertion and 2 min after that, which can be caused by the patient’s anxiety reduction after anesthesia induction, in addition to the proper time of LMA insertion. Zeinali et al. reported an increase in blood pressure and heart rate after LMA insertion and endotracheal intubation that continued and is probably due to insufficient anesthesia depth in the case of airway instrument placement or insufficient anesthetic dosing (17). The lack of significant differences in hemodynamic parameters between the two groups reinforces the safety and efficacy of both maneuvers. These results suggest that either maneuver can effectively determine the appropriate time for LMA insertion, reducing the risk of airway-related complications and optimizing anesthetic management.
The limitation of the present work is the small available sample size and the inclusion of only adult patients. The varied distribution of drugs in the pediatric population may lead to different results; therefore, studying the pediatric population with different drugs is recommended.
Conclusions
According to the results of this study, it is suggested that the mentors and students consider utilizing any of the mentioned maneuvers to determine the appropriate time of laryngeal mask insertion to prevent undesirable hemodynamic changes in the elderly or patients with cardiovascular comorbidities that can cause injury.
Acknowledgments
We would like to thank everyone who collaborated on this research.
Funding
The authors declare there were no funding sources for this work.
Conflict of Interest
The authors declare that there is no conflict of interest.
Type of Study: Research |
Subject:
Orthopedia
Received: 2025/01/5 | Accepted: 2025/02/2 | ePublished ahead of print: 2025/04/22 | Published: 2025/04/22
Received: 2025/01/5 | Accepted: 2025/02/2 | ePublished ahead of print: 2025/04/22 | Published: 2025/04/22
References
1. Goudra B, Singh PM. ERCP: the unresolved question of endotracheal intubation. Dig Dis Sci. 2014;59(3):513-519. [DOI:10.1007/s10620-013-2931-3]
2. Divatia J, Bhowmick K. Complications of endotracheal intubation and other airway management procedures. Indian J Anaesth. 2005;49(4): 308-318.
3. Kim CL, Lim H, Kang L, Kwon J, Jung Y, Jeong MA, et al. Comparison between the standard method and the 30° curved tongue depressor-aided technique for insertion of a laryngeal mask airway: a randomized controlled trial. BMC Anesthesiol. 2024;24(1):353. [DOI:10.1186/s12871-024-02741-0]
4. Gravningsbråten R, Nicklasson B, Raeder J. Safety of laryngeal mask airway and short-stay practice in office-based adenotonsillectomy. Acta Anaesthesiol Scand. 2009;53(2):218-222. [DOI:10.1111/j.1399-6576.2008.01806.x]
5. S Shetabi H, Shahriari A, Aghadavoudi O. Conditions for insertion of the laryngeal mask airway in an innovative method vs the classic method. Anesth Pain Med. 2023;13(6):e140999. [DOI:10.5812/aapm-140999]
6. Hagberg C, Georgi R, Krier C. Complications of managing the airway. Best Pract Res Clin Anaesthesiol. 2005;19(4):641-659. [DOI:10.1016/j.bpa.2005.08.002]
7. Chang CH, Shim YH, Shin YS, Lee KY. Optimal conditions for laryngeal mask airway insertion in children can be determined by the trapezius squeezing test. J Clin Anesth. 2008;20(2):99-102. [DOI:10.1016/j.jclinane.2007.09.007]
8. Devyani Desai J, Upadhyay MR, Prajapati A. Trapezius squeezetest versus jaw thrust to assess the depth of anaesthesia for proseal laryngeal mask airway insertion in children. J Anesth Crit Care. 2014;1(4): 00025. [DOI:10.15406/jaccoa.2014.01.00025]
9. Matta BF, Marsh DS, Nevin M. Laryngeal mask airway: a more successful method of insertion. J Clin Anesth. 1995;7(2):132-135. [DOI:10.1016/0952-8180(94)00027-2]
10. Asai T, Morris S. The laryngeal mask airway: its features, effects and role. Can J Anaesth. 1994;41(10):930-960. [DOI:10.1007/BF03010937]
11. Wan L, Shao LJ, Liu Y, Wang HX, Xue FS, Tian M. A feasibility study of jaw thrust as an indicator assessing adequate depth of anesthesia for insertion of supraglottic airway device in morbidly obese patients. Chin Med J (Engl). 2019;132(18):2185-2191. [DOI:10.1097/CM9.0000000000000403]
12. Scanlon P, Carey M, Power M, Kirby F. Patient response to laryngeal mask insertion after induction of ana esthesia with propofol or thiopentone. Can J Anaesth. 1993;40(9):816-818. [DOI:10.1007/BF03009250]
13. Chang CH, Kim SH, Shim YH, Kim JH, Shin YS. Comparison of the trapezius squeezing test and jaw thrust as indicators for laryngeal mask airway insertion in adults. Korean J Anesthesiol. 2011;61(3):201-204. [DOI:10.4097/kjae.2011.61.3.201]
14. Kouzegaran S, Allahyari E, Shakhsemampour BF, Sabertanha A, Hoseinian SM. Comparison between the efficacy of trapezius squeezing test and jaw thrust maneuver for prediction of successful insertion of laryngeal mask airway. J Urmia Univ Med Sci. 2019;30(2): 116-121.
15. Liu JZ, Zhao J, Zhang YJ. Comparison of jaw thrust and trapezius squeezing test as indicators for laryngeal mask airway insertion in infants and young children. Zhonghua Yi Xue Za Zhi, 2016. 96(6): 451-455.
16. Hooda S, Kaur K, Rattan KN, Thakur AK, Kamal K. Trapezius squeeze test as an indicator for depth of anesthesia for laryngeal mask airway insertion in children. J Anaesthesiol Clin Pharmacol. 2012;28(1): 28-31. [DOI:10.4103/0970-9185.92430]
17. Zeinali MB, Heshmati F, Abbasi Vash R, Beig Mohammadi MT. Comparative study of arterial blood pressure and heart rate changes due to laryngeal mask airway insertion vs endotracheal intubation after induction of anesthesia. J Iranian Soc Anaesthesiol Intensive Care. 2005;27(51): 15-21.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |