Volume 13, Issue 2 (6-2025)
J Surg Trauma 2025, 13(2): 84-86 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Amouzeshi A, Ganjifard M, Ansari Aval Z, Shakhs Emempour B F, Bahramian M, Bahramian M, et al . Report of a Supportive Care Case during Cardiopulmonary Bypass in a Patient with a History of Infective Endocarditis Causing Multiple Embolic Cerebral Infarctions with Hemorrhagic Transformation. J Surg Trauma 2025; 13 (2) :84-86
URL: http://jsurgery.bums.ac.ir/article-1-480-en.html
URL: http://jsurgery.bums.ac.ir/article-1-480-en.html
Ahmad Amouzeshi 

 , Mahmoud Ganjifard
, Mahmoud Ganjifard 

 , Zahra Ansari Aval
, Zahra Ansari Aval 

 , Bibi Fatemeh Shakhs Emempour
, Bibi Fatemeh Shakhs Emempour 

 , Maryam Bahramian
, Maryam Bahramian 

 , Mozhgan Bahramian
, Mozhgan Bahramian 

 , Nafiseh Sadat Haerizadeh
, Nafiseh Sadat Haerizadeh 

 , Seyyed Ebrahim Hosseini Zargaz *
, Seyyed Ebrahim Hosseini Zargaz * 




 , Mahmoud Ganjifard
, Mahmoud Ganjifard 

 , Zahra Ansari Aval
, Zahra Ansari Aval 

 , Bibi Fatemeh Shakhs Emempour
, Bibi Fatemeh Shakhs Emempour 

 , Maryam Bahramian
, Maryam Bahramian 

 , Mozhgan Bahramian
, Mozhgan Bahramian 

 , Nafiseh Sadat Haerizadeh
, Nafiseh Sadat Haerizadeh 

 , Seyyed Ebrahim Hosseini Zargaz *
, Seyyed Ebrahim Hosseini Zargaz * 


Cardiovascular Diseases Research Center, Birjand University of Medical Sciences, Birjand, Iran
Full-Text [PDF 335 kb]
(168 Downloads)
| Abstract (HTML) (472 Views)
Discussion
There is a wide range of heart diseases that require surgical intervention, including coronary artery bypass grafting and heart valve replacement. Mitral valve endocarditis can be caused by various pathogens; however, bacterial origin is the most common in developed countries (3, 4). Infective endocarditis (IE) is one of the most common causes of acute mitral valve regurgitation. IE poses a significant risk for vascular complications, including cerebral embolism, ICH, and aneurysms, which are associated with high mortality rates. While anticoagulant therapy is one of the main strategies for managing thromboembolic complications, its application in IE patients remains challenging and debated. The incidence of stroke in individuals with IE is estimated to be around 10%, primarily due to embolic regions or bleeding. Ischemic strokes are generally more common than cerebral hemorrhages. ICHs in uncontrolled infections typically occur due to septic emboli and the formation of mycotic aneurysms, often resulting from delayed initiation of antibiotic treatment (1). In the case we reported, the patient also experienced cerebral hemorrhage, suspected to stem from uncontrolled infection due to endocarditis. One of the anticoagulants used during cardiopulmonary bypass is heparin, which is administered at a dose of 300-400 units per kilogram during anesthesia and 100 units during cardiopulmonary bypass to maintain a minimum clotting time of 400 to 480 seconds. We aimed to keep the ACT within the minimum normal range of 400 (5). Another strategy we employed in this patient was the use of alpha stat technique, which provided advantages over the pH-stat technique, with both methods maintaining a normal pH. In the alpha technique, pH is maintained at 37 degrees, while in the pH-stat method, the patient's actual temperature pH is preserved. The alpha technique is preferable for adults and patients with normothermia and mild hypothermia, reducing the risk of embolization, compared to pH-stat. Thus, considering the increased risk of cerebral perfusion and embolization, we utilized the alpha stat technique alongside ice packs to reduce metabolic brain demand and enhance cooling speed. Another strategy applied in these patients was tranexamic acid, administered at 30 mg per kilogram. Previous studies have indicated that tranexamic acid reduces the risk of cerebral hemorrhage and improves neurological function (6-8). In our case, the patient was discharged after surgery without exacerbation of cerebral hemorrhagic conditions.
Conclusions
The incidence of embolism and the development of cerebral hemorrhage in patients with endocarditis, although rare, can occur if endocarditis is not treated promptly with antibiotic therapy, leading to cerebral hemorrhage. A specific strategy during cardiopulmonary bypass has not yet been reported in these patients; however, based on our experience with this case, surgical intervention can be performed with minimal complications. The alpha stat technique, tranexamic acid administration, and minimum ACT maintenance are among the most crucial strategies.
Conflict of Interest
The authors declare no conflict of interest for this manuscript.
Full-Text: (100 Views)
Abstract
The occurrence of cerebral embolic infarct following endocarditis is a complication that can lead to serious outcomes and mortality. The present case involves a patient with a history of intravenous drug use who developed multiple septic emboli and subsequent cerebral hemorrhage due to endocarditis. The patient was urgently scheduled for valve replacement surgery. Considering the patient's specific condition and history of hemorrhagic stroke, supportive measures during cardiopulmonary bypass were implemented without any specific complications, and the patient was discharged from the hospital after one week. Performing valve replacement surgeries in patients with a previous history of hemorrhagic stroke can be dangerous due to complications arising from anticoagulation, inflammatory responses, and changes in cerebral perfusion flow, potentially leading to death. However, these complications can be effectively mitigated with a series of supportive measures during cardiopulmonary bypass.
Key words: Bypass Endocarditis, Cardiopulmonary, Cerebral Hemorrhage
Introduction
Endocarditis is one of the major causes of cardiac embolism and carries a high rate of morbidity and mortality. A study published in 2020 indicated that the annual incidence of endocarditis ranges from 3 to 10 cases per 100,000 people, with a 30-day mortality rate remaining high at about 30%. There are three main types of endocarditis, namely infective endocarditis (IE), non-bacterial thrombotic endocarditis, and Libman-sacks endocarditis. IE is the most common type, while malignancies are usually associated with non-bacterial thrombotic endocarditis, and patients with systemic lupus erythematosus and antiphospholipid syndrome frequently exhibit Libman-sacks endocarditis. Unfortunately, embolism diagnosis is often delayed, underscoring the necessity for timely identification and intervention (1).
Systemic embolization can occur with IE, with the brain and spleen being the most common sites in left-sided IE. The occurrence of embolic events in the central nervous system is noted in 25% to 40% of cases and is associated with poor outcomes. Cerebral infarcts have a high risk of hemorrhagic transformation, especially with high doses of anticoagulants used during cardiopulmonary bypass, which increase the risk of intracranial hemorrhage (ICH) during surgery (2). The present case is of a patient who presented with ICH before surgery and was considered for mitral valve replacement following endocarditis.
Case
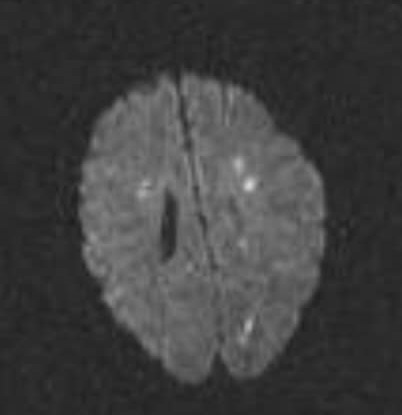
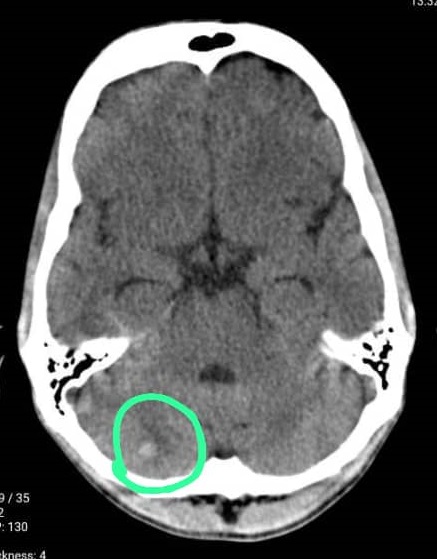
The patient was a 25-year-old male with a history of intravenous drug abuse who presented to the hospital with a mild fever and chills over the past week. The patient had experienced one episode of seizures. CT scans of the brain revealed multiple septic emboli. The patient was treated with apotel, vancomycin, meropenem, and levetiracetam, which were administered at varying frequencies. The patient's history included addiction to crystal meth and methadone, along with nausea and vomiting. Additionally, the patient had a history of alcohol and hookah use. Diffusion-weighted MRI images (DWI) demonstrated multiple acute small infarcts scattered in different vascular territories of bilateral cerebral hemispheres, which is the typical pattern of embolic infarct (Figure 1). Axial brain CT showed cerebellar infarct with hemorrhagic transformation, that is a common feature of embolic infarcts (Figure 2). Echocardiography revealed severe mitral regurgitation and pulmonary artery pressure between 50 and 55. The echocardiographic findings were highly indicative of IE of the mitral valve, leading to severe mitral regurgitation and left ventricular dysfunction. A large vegetation measuring 3×3 cm was also noted in the left atrium. The patient was emergently placed in the cardiac surgery unit, and 300 units of heparin per kilogram were administered before cannulation, with an additional 5000 units of heparin given during bypass. The activated clotting time was maintained in an acceptable minimum range of 400 to 450 to reduce the anticoagulant infusion and prevent worsening of ICH and associated brain complications. Tranexamic acid was also administered at 30 mg per kilogram, resulting in a total dose of 1500 mg. The patient underwent moderate hypothermia, cooling to 28 degrees, with a cross-clamp time of 97 minutes and a pump time of 108 minutes. A mechanical mitral valve of size 31 was implanted. As the patient was subjected to moderate hypothermia and considering the hemorrhagic areas in the brain, the alpha technique was utilized to reduce cerebral perfusion pressure and the risk of embolization. Ultimately, the patient was transferred to the intensive care unit and then to the general ward, being discharged after seven days.
The occurrence of cerebral embolic infarct following endocarditis is a complication that can lead to serious outcomes and mortality. The present case involves a patient with a history of intravenous drug use who developed multiple septic emboli and subsequent cerebral hemorrhage due to endocarditis. The patient was urgently scheduled for valve replacement surgery. Considering the patient's specific condition and history of hemorrhagic stroke, supportive measures during cardiopulmonary bypass were implemented without any specific complications, and the patient was discharged from the hospital after one week. Performing valve replacement surgeries in patients with a previous history of hemorrhagic stroke can be dangerous due to complications arising from anticoagulation, inflammatory responses, and changes in cerebral perfusion flow, potentially leading to death. However, these complications can be effectively mitigated with a series of supportive measures during cardiopulmonary bypass.
Key words: Bypass Endocarditis, Cardiopulmonary, Cerebral Hemorrhage
Introduction
Endocarditis is one of the major causes of cardiac embolism and carries a high rate of morbidity and mortality. A study published in 2020 indicated that the annual incidence of endocarditis ranges from 3 to 10 cases per 100,000 people, with a 30-day mortality rate remaining high at about 30%. There are three main types of endocarditis, namely infective endocarditis (IE), non-bacterial thrombotic endocarditis, and Libman-sacks endocarditis. IE is the most common type, while malignancies are usually associated with non-bacterial thrombotic endocarditis, and patients with systemic lupus erythematosus and antiphospholipid syndrome frequently exhibit Libman-sacks endocarditis. Unfortunately, embolism diagnosis is often delayed, underscoring the necessity for timely identification and intervention (1).
Systemic embolization can occur with IE, with the brain and spleen being the most common sites in left-sided IE. The occurrence of embolic events in the central nervous system is noted in 25% to 40% of cases and is associated with poor outcomes. Cerebral infarcts have a high risk of hemorrhagic transformation, especially with high doses of anticoagulants used during cardiopulmonary bypass, which increase the risk of intracranial hemorrhage (ICH) during surgery (2). The present case is of a patient who presented with ICH before surgery and was considered for mitral valve replacement following endocarditis.
Case
The patient was a 25-year-old male with a history of intravenous drug abuse who presented to the hospital with a mild fever and chills over the past week. The patient had experienced one episode of seizures. CT scans of the brain revealed multiple septic emboli. The patient was treated with apotel, vancomycin, meropenem, and levetiracetam, which were administered at varying frequencies. The patient's history included addiction to crystal meth and methadone, along with nausea and vomiting. Additionally, the patient had a history of alcohol and hookah use. Diffusion-weighted MRI images (DWI) demonstrated multiple acute small infarcts scattered in different vascular territories of bilateral cerebral hemispheres, which is the typical pattern of embolic infarct (Figure 1). Axial brain CT showed cerebellar infarct with hemorrhagic transformation, that is a common feature of embolic infarcts (Figure 2). Echocardiography revealed severe mitral regurgitation and pulmonary artery pressure between 50 and 55. The echocardiographic findings were highly indicative of IE of the mitral valve, leading to severe mitral regurgitation and left ventricular dysfunction. A large vegetation measuring 3×3 cm was also noted in the left atrium. The patient was emergently placed in the cardiac surgery unit, and 300 units of heparin per kilogram were administered before cannulation, with an additional 5000 units of heparin given during bypass. The activated clotting time was maintained in an acceptable minimum range of 400 to 450 to reduce the anticoagulant infusion and prevent worsening of ICH and associated brain complications. Tranexamic acid was also administered at 30 mg per kilogram, resulting in a total dose of 1500 mg. The patient underwent moderate hypothermia, cooling to 28 degrees, with a cross-clamp time of 97 minutes and a pump time of 108 minutes. A mechanical mitral valve of size 31 was implanted. As the patient was subjected to moderate hypothermia and considering the hemorrhagic areas in the brain, the alpha technique was utilized to reduce cerebral perfusion pressure and the risk of embolization. Ultimately, the patient was transferred to the intensive care unit and then to the general ward, being discharged after seven days.
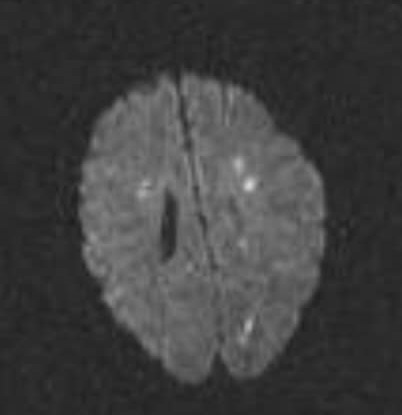
Figure1. MRI, Diffusion-Weighted Image, Restricted Diffusion Foci on DWI
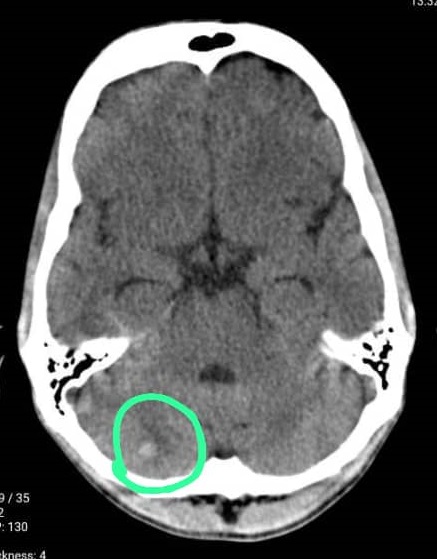
Figure2. Axial Brain CT, Cerebellar Infarct with Hemorrhagic Transformation
Discussion
There is a wide range of heart diseases that require surgical intervention, including coronary artery bypass grafting and heart valve replacement. Mitral valve endocarditis can be caused by various pathogens; however, bacterial origin is the most common in developed countries (3, 4). Infective endocarditis (IE) is one of the most common causes of acute mitral valve regurgitation. IE poses a significant risk for vascular complications, including cerebral embolism, ICH, and aneurysms, which are associated with high mortality rates. While anticoagulant therapy is one of the main strategies for managing thromboembolic complications, its application in IE patients remains challenging and debated. The incidence of stroke in individuals with IE is estimated to be around 10%, primarily due to embolic regions or bleeding. Ischemic strokes are generally more common than cerebral hemorrhages. ICHs in uncontrolled infections typically occur due to septic emboli and the formation of mycotic aneurysms, often resulting from delayed initiation of antibiotic treatment (1). In the case we reported, the patient also experienced cerebral hemorrhage, suspected to stem from uncontrolled infection due to endocarditis. One of the anticoagulants used during cardiopulmonary bypass is heparin, which is administered at a dose of 300-400 units per kilogram during anesthesia and 100 units during cardiopulmonary bypass to maintain a minimum clotting time of 400 to 480 seconds. We aimed to keep the ACT within the minimum normal range of 400 (5). Another strategy we employed in this patient was the use of alpha stat technique, which provided advantages over the pH-stat technique, with both methods maintaining a normal pH. In the alpha technique, pH is maintained at 37 degrees, while in the pH-stat method, the patient's actual temperature pH is preserved. The alpha technique is preferable for adults and patients with normothermia and mild hypothermia, reducing the risk of embolization, compared to pH-stat. Thus, considering the increased risk of cerebral perfusion and embolization, we utilized the alpha stat technique alongside ice packs to reduce metabolic brain demand and enhance cooling speed. Another strategy applied in these patients was tranexamic acid, administered at 30 mg per kilogram. Previous studies have indicated that tranexamic acid reduces the risk of cerebral hemorrhage and improves neurological function (6-8). In our case, the patient was discharged after surgery without exacerbation of cerebral hemorrhagic conditions.
Conclusions
The incidence of embolism and the development of cerebral hemorrhage in patients with endocarditis, although rare, can occur if endocarditis is not treated promptly with antibiotic therapy, leading to cerebral hemorrhage. A specific strategy during cardiopulmonary bypass has not yet been reported in these patients; however, based on our experience with this case, surgical intervention can be performed with minimal complications. The alpha stat technique, tranexamic acid administration, and minimum ACT maintenance are among the most crucial strategies.
Conflict of Interest
The authors declare no conflict of interest for this manuscript.
Type of Study: Case Report |
Subject:
Heart Surgery
Received: 2025/05/16 | Accepted: 2025/06/9 | ePublished ahead of print: 2025/06/17 | Published: 2025/06/17
Received: 2025/05/16 | Accepted: 2025/06/9 | ePublished ahead of print: 2025/06/17 | Published: 2025/06/17
References
1. Pham S, Heigle B, Gibbs C, Gebrehiwot WG, Pannu P. Complications of infective endocarditis: A case report of intracerebral hemorrhage exacerbated by enoxaparin. Cureus. 2024;16(5):e61235. [DOI:10.7759/cureus.61235]
2. Kesieme EB, Omoregbee B, Ngaage DL. A case report supporting early surgery in mitral valve infective endocarditis with recurrent cerebral infarcts. Eur Heart J Case Rep. 2024;8(12): ytae64. [DOI:10.1093/ehjcr/ytae641]
3. Amouzeshi A, Zargaz SE, Rezaei M, Riahi SM, Sa'adat F. The comparison of postoperative complications in hypothyroid and euthyroid patients undergoing cardiac surgery: A retrospective cohort study. Int Cardiovascu Res J. 2023;17(1):24-30.
4. Nappi F, Spadaccio C, Dreyfus J, Attias D, Acar C, Bando K. Mitral endocarditis: A new management framework. J Thorac Cardiovasc Surg. 2018;156(4):1486-95. [DOI:10.1016/j.jtcvs.2018.03.159]
5. Cartwright B, Mundell N. Anticoagulation for cardiopulmonary bypass: part one. BJA Educ. 2023;23(3):110-6. [DOI:10.1016/j.bjae.2022.12.003]
6. McKinley WI, Rowell SE, Mansour A, Hoefer L, Polcari A, Schreiber M, et al. Tranexamic acid, mortality, and intracranial hemorrhage type in moderate or severe traumatic brain injury. JAMA Surg. 2023;158(11):1222-4. [DOI:10.1001/jamasurg.2023.3848]
7. Hu W, Xin Y, Chen X, Song Z, He Z, Zhao Y. Tranexamic acid in cerebral hemorrhage: a meta-analysis and systematic review. CNS Drugs. 2019; 33:327-36. [DOI:10.1007/s40263-019-00608-4]
8. Xiong Y, Guo X, Huang X, Kang X, Zhou J, Chen C, et al. Efficacy and safety of tranexamic acid in intracranial haemorrhage: A meta-analysis. PLoS One. 2023;18(3):e0282726. [DOI:10.1371/journal.pone.0282726]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |