Volume 14, Issue 1 (1-2026)
J Surg Trauma 2026, 14(1): 46-50 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Abdoli Tafti A, Gholizadeh M. Distal Humerus Physeal Separation in a Neonate: A Case Report. J Surg Trauma 2026; 14 (1) :46-50
URL: http://jsurgery.bums.ac.ir/article-1-479-en.html
URL: http://jsurgery.bums.ac.ir/article-1-479-en.html
Department of Orthopedic Surgery, Trauma Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran
Full-Text [PDF 491 kb]
(179 Downloads)
| Abstract (HTML) (588 Views)
.png)
.png)
Figure 2. Radiographs at 16 Days after birth with Early Callus Formation (one week after trauma)
Figure 3. Radiographs at 60 Days Showing Healing

2(.jpg)




Full-Text: (181 Views)
Abstract
Distal humerus physeal separation is a rare and often underdiagnosed injury in neonates, typically associated with birth trauma or child abuse. We present a case of a 9-day-old neonate with a Salter-Harris type I physeal separation of the distal humerus, managed conservatively due to delayed presentation. Long-term follow-up over 4 years demonstrated excellent remodeling and full elbow function despite the absence of early reduction. This case highlights the potential for favorable outcomes with conservative management in cases of delayed diagnosis, contributing to the limited existing literature on this condition.
Key words: Distal humeral fracture, Infant, Newborn, Slipped epiphyses
Distal humerus physeal separation is a rare and often underdiagnosed injury in neonates, typically associated with birth trauma or child abuse. We present a case of a 9-day-old neonate with a Salter-Harris type I physeal separation of the distal humerus, managed conservatively due to delayed presentation. Long-term follow-up over 4 years demonstrated excellent remodeling and full elbow function despite the absence of early reduction. This case highlights the potential for favorable outcomes with conservative management in cases of delayed diagnosis, contributing to the limited existing literature on this condition.
Key words: Distal humeral fracture, Infant, Newborn, Slipped epiphyses
Introduction
Elbow injuries are a frequent cause of pediatric emergency department visits. Diagnosing these injuries in young patients can be particularly challenging due to difficulties in obtaining a comprehensive medical history and conducting a thorough clinical examination. Cooperation issues during radiographic assessments further complicate the situation, as interpreting these images is often hindered by the cartilaginous composition of certain bones in the elbow area. Distal humeral physeal separation, although rare, is frequently overlooked and typically occurs in children younger than two years, representing approximately 1.6% of pediatric distal humeral fractures (1, 2, 3). Smith first identified this condition in 1850 (3). The injury usually results from a fall onto an outstretched hand or hyperextension combined with significant rotation of the elbow and forearm (2).
Birth trauma is a notable cause of this condition, often becoming apparent a few days post-delivery (2, 4). Contributing risk factors include challenging deliveries, abnormal fetal positioning, macrosomia, and cephalopelvic disproportion (5). Additionally, child abuse is a recognized cause of physeal separation, with approximately 50% of cases in children under two being linked to such abuse. A thorough medical history, comprehensive physeal examination, and a high index of suspicion are crucial for accurate diagnosis (2, 3).
The clinical manifestations of this condition include swelling around the elbow, tenderness, restlessness, and reduced range of motion (ROM) (4). During physeal examination, preserving the posterior triangle of the elbow can help distinguish physeal separation from an elbow dislocation (3). The characteristic muffled crepitus sign occurs when the two cartilaginous surfaces move against each other (6).
Radiography is the primary method for diagnosing this condition. In infants younger than 8 months, the distal humeral epiphysis is often still cartilaginous due to the ongoing development of the capitellum's ossification center. On radiographic images, physeal separation can be confused with elbow dislocation. A notable radiological indicator of distal humeral physis injury is posteromedial displacement of the radio-ulnar complex (5). Other significant radiological findings include distal humeral metaphyseal fragments, a displaced medial epicondyle, and a displaced ossification center of the capitellum (7).
Ultrasound is also a valuable diagnostic option in these scenarios, although its effectiveness depends on the operator's skill (2, 3). It can reveal the displacement of the non-ossified distal humeral epiphysis, as well as the presence of effusion and extra-articular issues (7). Arthrography can provide detailed insights into cartilage damage and fracture assessment; however, it is an invasive procedure with a risk of infection and is not typically recommended for routine use. Magnetic resonance imaging (MRI) is useful for identifying physeal injuries; however, its drawbacks include the need for anesthesia and its high cost (5).
Alongside elbow dislocation, other differential diagnoses for physeal separation include septic arthritis, osteomyelitis, brachial plexus injury, and genetic conditions such as osteogenesis imperfecta (2). Posteromedial displacement is more frequently observed than posterolateral displacement, and anterior displacement is relatively uncommon (3).
This type of injury is treated more conservatively (2). The timing of fracture detection plays a crucial role in determining the appropriate treatment method. If diagnosed early, the preferred treatment involves closed reduction followed by immobilization with a splint. If the diagnosis is delayed beyond 5-7 days, manipulation of the fracture is not recommended, and treatment will proceed with splinting and casting (5, 8). If signs of instability are observed after reduction, percutaneous pinning is performed using two lateral pins for stabilization. If the stress test indicates stability after the first pin is placed, the second pin can be added to prevent rotational movement. Caution is advised to avoid pinning from the medial side due to the risk of ulnar nerve injury (4). Cubitus varus is the most frequently observed complication associated with physeal separation (2). Osteonecrosis, non-:union:, and neurovascular complications are relatively rare (3).
This study presents a case of distal humeral physeal separation in a neonate. Despite delayed presentation, conservative treatment led to favorable long-term outcomes.
Case presentation
A 9-day-old term neonate, born via uncomplicated vaginal delivery, presented with restricted movement of the right upper limb. Although discharged without issues per medical records, the parents reported symptom onset from birth. Examination revealed elbow swelling, tenderness, and reduced ROM, with intact neurovascular status and a preserved posterior elbow triangle. Laboratory tests showed no infection. Anteroposterior (AP) and lateral radiographs (Figure 1) demonstrated posteromedial displacement of the radio-ulnar complex, consistent with a Salter-Harris type I distal humerus physeal separation. Due to delayed presentation, closed reduction was not attempted, and the elbow was immobilized with a splint. One week later, radiographs showed early callus formation (Figure 2).
Elbow injuries are a frequent cause of pediatric emergency department visits. Diagnosing these injuries in young patients can be particularly challenging due to difficulties in obtaining a comprehensive medical history and conducting a thorough clinical examination. Cooperation issues during radiographic assessments further complicate the situation, as interpreting these images is often hindered by the cartilaginous composition of certain bones in the elbow area. Distal humeral physeal separation, although rare, is frequently overlooked and typically occurs in children younger than two years, representing approximately 1.6% of pediatric distal humeral fractures (1, 2, 3). Smith first identified this condition in 1850 (3). The injury usually results from a fall onto an outstretched hand or hyperextension combined with significant rotation of the elbow and forearm (2).
Birth trauma is a notable cause of this condition, often becoming apparent a few days post-delivery (2, 4). Contributing risk factors include challenging deliveries, abnormal fetal positioning, macrosomia, and cephalopelvic disproportion (5). Additionally, child abuse is a recognized cause of physeal separation, with approximately 50% of cases in children under two being linked to such abuse. A thorough medical history, comprehensive physeal examination, and a high index of suspicion are crucial for accurate diagnosis (2, 3).
The clinical manifestations of this condition include swelling around the elbow, tenderness, restlessness, and reduced range of motion (ROM) (4). During physeal examination, preserving the posterior triangle of the elbow can help distinguish physeal separation from an elbow dislocation (3). The characteristic muffled crepitus sign occurs when the two cartilaginous surfaces move against each other (6).
Radiography is the primary method for diagnosing this condition. In infants younger than 8 months, the distal humeral epiphysis is often still cartilaginous due to the ongoing development of the capitellum's ossification center. On radiographic images, physeal separation can be confused with elbow dislocation. A notable radiological indicator of distal humeral physis injury is posteromedial displacement of the radio-ulnar complex (5). Other significant radiological findings include distal humeral metaphyseal fragments, a displaced medial epicondyle, and a displaced ossification center of the capitellum (7).
Ultrasound is also a valuable diagnostic option in these scenarios, although its effectiveness depends on the operator's skill (2, 3). It can reveal the displacement of the non-ossified distal humeral epiphysis, as well as the presence of effusion and extra-articular issues (7). Arthrography can provide detailed insights into cartilage damage and fracture assessment; however, it is an invasive procedure with a risk of infection and is not typically recommended for routine use. Magnetic resonance imaging (MRI) is useful for identifying physeal injuries; however, its drawbacks include the need for anesthesia and its high cost (5).
Alongside elbow dislocation, other differential diagnoses for physeal separation include septic arthritis, osteomyelitis, brachial plexus injury, and genetic conditions such as osteogenesis imperfecta (2). Posteromedial displacement is more frequently observed than posterolateral displacement, and anterior displacement is relatively uncommon (3).
This type of injury is treated more conservatively (2). The timing of fracture detection plays a crucial role in determining the appropriate treatment method. If diagnosed early, the preferred treatment involves closed reduction followed by immobilization with a splint. If the diagnosis is delayed beyond 5-7 days, manipulation of the fracture is not recommended, and treatment will proceed with splinting and casting (5, 8). If signs of instability are observed after reduction, percutaneous pinning is performed using two lateral pins for stabilization. If the stress test indicates stability after the first pin is placed, the second pin can be added to prevent rotational movement. Caution is advised to avoid pinning from the medial side due to the risk of ulnar nerve injury (4). Cubitus varus is the most frequently observed complication associated with physeal separation (2). Osteonecrosis, non-:union:, and neurovascular complications are relatively rare (3).
This study presents a case of distal humeral physeal separation in a neonate. Despite delayed presentation, conservative treatment led to favorable long-term outcomes.
Case presentation
A 9-day-old term neonate, born via uncomplicated vaginal delivery, presented with restricted movement of the right upper limb. Although discharged without issues per medical records, the parents reported symptom onset from birth. Examination revealed elbow swelling, tenderness, and reduced ROM, with intact neurovascular status and a preserved posterior elbow triangle. Laboratory tests showed no infection. Anteroposterior (AP) and lateral radiographs (Figure 1) demonstrated posteromedial displacement of the radio-ulnar complex, consistent with a Salter-Harris type I distal humerus physeal separation. Due to delayed presentation, closed reduction was not attempted, and the elbow was immobilized with a splint. One week later, radiographs showed early callus formation (Figure 2).
.png)
Figure 1. Anteroposterior (AP) and Lateral Radiographs at 9 Days Showing Posteromedial Radio-Ulnar Displacement
.png)
Figure 2. Radiographs at 16 Days after birth with Early Callus Formation (one week after trauma)
At follow-up three weeks later, the patient's splint was removed. The patient was revisited 50 days later, with radiographs indicating healing (Figure 3) and near-normal ROM despite mild varus (Figure 4). At 4-year follow-up, the patient was pain-free, with normal ROM (Figure 5) and radiographic evidence of complete remodeling (Figure 6), without physeal bar formation or deformity. Over the past four years, the patient has been able to perform daily activities without issues and has not required specific medical care. Notably, the mother later disclosed an unintentional injury by the father, not birth trauma, explaining the delayed referral. Informed consent was obtained for this report.
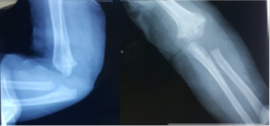
Figure 3. Radiographs at 60 Days Showing Healing

2(.jpg)
Figure 4. Range of Motion (ROM) at 60 Days with Mild Varus of right elbow




Figure 5. Normal Range of Motion (ROM) at 4 Years
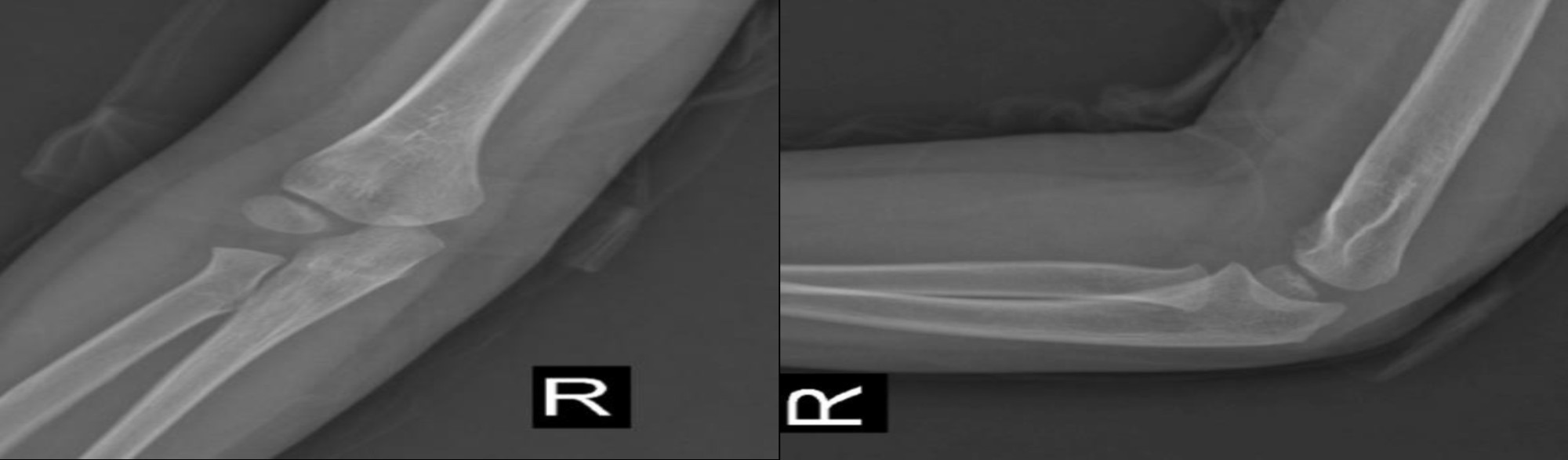
Figure 6. Radiographs at 4 Years with Complete Remodeling
Discussion
Distal humerus physeal separation is rare, often linked to birth trauma, difficult deliveries (e.g., macrosomia), or child abuse, with the latter implicated in approximately 50% of cases under 2 years (2). Clinical features include elbow swelling, tenderness, and muffled crepitus, with an intact posterior triangle distinguishing it from dislocation (3). Radiographs may mimic dislocation due to cartilaginous epiphyses in neonates, though posteromedial radio-ulnar displacement is diagnostic (5). Ultrasound, arthrography, and MRI aid diagnosis but vary in feasibility (7).
Treatment hinges on timing: early closed reduction with splinting is preferred, while delays beyond 5-7 days favor immobilization alone (4). Pinning is reserved for cases of instability, as it avoids medial approaches due to the risk of ulnar nerve injury (8). Cubitus varus is the most common complication (2).
Our case aligns with prior reports but stands out for its etiology (unintentional parental trauma) and management. Malik et al. described a neonate with physeal separation post-cesarean, initially misdiagnosed as a dislocation, treated with splinting, and showing mild varus at 2 months (5). Kamaci et al. reported full ROM 6 months after early reduction and pinning (4). In contrast, our patient, who was untreated due to a delay, achieved excellent 4-year outcomes with conservative care alone. Although a degree of cubitus varus was present in this case, it did not result in any functional impairment. This suggests that in neonates with delayed presentation, remodeling potential may mitigate the need for early intervention, challenging conventional approaches, and highlighting the need for further comparative studies in the future.
Conclusions
This case highlights the diagnostic challenges and therapeutic considerations of distal humerus physeal separation in neonates, particularly in cases of delayed diagnosis. Despite a delay in diagnosis, conservative management was employed in this case, resulting in excellent long-term outcomes after four years, demonstrating the remarkable remodeling capacity of neonatal bones. During this period, the patient performed daily activities without issues and required no specific medical interventions, indicating stable recovery and functional preservation. However, the involved side had more varus compared to the contralateral side, which did not impair function. Clinicians should maintain a high index of suspicion for this injury in atypical presentations and consider conservative treatment options when timely reduction is not feasible, while ensuring long-term monitoring to assess potential complications such as cubitus varus.
Ethics Approval and Consent to Participate
Our Institutional Review Board approved this study. Written informed consent was obtained from the patient's parents for participation in this case report and for publication of the accompanying images.
Consent for Publication
Written informed consent for publication of this case report and any accompanying images was obtained from the patient's parents.
Data Availability Statement
The data supporting the findings of this case report are available from the corresponding author upon reasonable request.
Funding Statement
No funding was received for conducting this case report.
Acknowledgements
None.
Authors’ Contribution
AAT contributed to conceptualization, patient management, and review & editing. MGh performed the literature review, data collection from medical records, and writing - review & editing. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest.
Declaration of generative AI in scientific writing
No generative AI technologies were used during the preparation of this manuscript.
Distal humerus physeal separation is rare, often linked to birth trauma, difficult deliveries (e.g., macrosomia), or child abuse, with the latter implicated in approximately 50% of cases under 2 years (2). Clinical features include elbow swelling, tenderness, and muffled crepitus, with an intact posterior triangle distinguishing it from dislocation (3). Radiographs may mimic dislocation due to cartilaginous epiphyses in neonates, though posteromedial radio-ulnar displacement is diagnostic (5). Ultrasound, arthrography, and MRI aid diagnosis but vary in feasibility (7).
Treatment hinges on timing: early closed reduction with splinting is preferred, while delays beyond 5-7 days favor immobilization alone (4). Pinning is reserved for cases of instability, as it avoids medial approaches due to the risk of ulnar nerve injury (8). Cubitus varus is the most common complication (2).
Our case aligns with prior reports but stands out for its etiology (unintentional parental trauma) and management. Malik et al. described a neonate with physeal separation post-cesarean, initially misdiagnosed as a dislocation, treated with splinting, and showing mild varus at 2 months (5). Kamaci et al. reported full ROM 6 months after early reduction and pinning (4). In contrast, our patient, who was untreated due to a delay, achieved excellent 4-year outcomes with conservative care alone. Although a degree of cubitus varus was present in this case, it did not result in any functional impairment. This suggests that in neonates with delayed presentation, remodeling potential may mitigate the need for early intervention, challenging conventional approaches, and highlighting the need for further comparative studies in the future.
Conclusions
This case highlights the diagnostic challenges and therapeutic considerations of distal humerus physeal separation in neonates, particularly in cases of delayed diagnosis. Despite a delay in diagnosis, conservative management was employed in this case, resulting in excellent long-term outcomes after four years, demonstrating the remarkable remodeling capacity of neonatal bones. During this period, the patient performed daily activities without issues and required no specific medical interventions, indicating stable recovery and functional preservation. However, the involved side had more varus compared to the contralateral side, which did not impair function. Clinicians should maintain a high index of suspicion for this injury in atypical presentations and consider conservative treatment options when timely reduction is not feasible, while ensuring long-term monitoring to assess potential complications such as cubitus varus.
Ethics Approval and Consent to Participate
Our Institutional Review Board approved this study. Written informed consent was obtained from the patient's parents for participation in this case report and for publication of the accompanying images.
Consent for Publication
Written informed consent for publication of this case report and any accompanying images was obtained from the patient's parents.
Data Availability Statement
The data supporting the findings of this case report are available from the corresponding author upon reasonable request.
Funding Statement
No funding was received for conducting this case report.
Acknowledgements
None.
Authors’ Contribution
AAT contributed to conceptualization, patient management, and review & editing. MGh performed the literature review, data collection from medical records, and writing - review & editing. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that they have no conflict of interest.
Declaration of generative AI in scientific writing
No generative AI technologies were used during the preparation of this manuscript.
Type of Study: Case Report |
Subject:
Orthopedia
Received: 2025/05/15 | Accepted: 2025/09/23 | ePublished ahead of print: 2025/10/29 | Published: 2025/12/27
Received: 2025/05/15 | Accepted: 2025/09/23 | ePublished ahead of print: 2025/10/29 | Published: 2025/12/27
References
1. Cheong WL, Kamisan N, Ismail II. Distal Humerus Physeal Separation: Diagnostic Challenges and Implications. Cureus. 2024;16(12):e76248. [DOI:10.7759/cureus.76248]
2. Siddiqui YS, Abbas MB, Anwer A, Abbas M, Chowdhry M, Khurana S.Bilateral distal humeral physeal separation--from birth trauma to family trauma. J Orthop Case Rep. 2023;13(9):88-92. [DOI:10.13107/jocr.2023.v13.i09.3888]
3. Mathew DK, Gangadharan S, Krishnamoorthy V, Shanmughanathan R. Anterior physeal separation of distal humerus. Indian J Orthop. 2021;55(1):208-12. [DOI:10.1007/s43465-020-00111-9]
4. Kamaci S, Danisman M, Marangoz S. Neonatal physeal separation of distal humerus during cesarean section. Am J Orthop. 2014;43(11):279-81.
5. Malik S, Khopkar SR, Korday CS, Jadhav SS, Bhaskar AR. Transphyseal injury of distal humerus. J Clin Diagn Res. 2015;9(11):1-2.
6. Gigante C, Kini SG, Origo C, Volpin A. Transphyseal separation of the distal humerus in newborns. Chin J Traumatol. 2017;20(3):183-6. [DOI:10.1016/j.cjtee.2017.04.003]
7. Hariharan AR, Nugraha HK, Ho CA, Bauer A, Mehlman CT, Sponseller PD, et al. Transphyseal Humeral Separations: An Often-Missed Fracture. Children (Basel). 2023;10(10):1716. [DOI:10.3390/children10101716]
8. Rockwood CA. Distal humeral physeal, medial condyle, lateral epicondylar, and other uncommon elbow fractures. In: Rockwood CA, editor. Rockwood and Wilkins' Fractures in Children. Philadelphia: Lippincott Williams & Wilkins; 2025. Chapter 18.
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







