Volume 13, Issue 3 (9-2025)
J Surg Trauma 2025, 13(3): 96-102 |
Back to browse issues page
Ethics code: IR.BUMS.REC.1400.324
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Zangoue M, Sharafi S, Shaarbaf Yazdi A, Tolyat M. Comparison of the Effects of Melatonin and Midazolam on Hemodynamic Status in Patients Candidate for Cataract Surgery: A Randomized Controlled Clinical Trial. J Surg Trauma 2025; 13 (3) :96-102
URL: http://jsurgery.bums.ac.ir/article-1-483-en.html
URL: http://jsurgery.bums.ac.ir/article-1-483-en.html
School of Allied Medical Sciences. Birjand University of Medical Sciences, Birjand, Iran
Full-Text [PDF 580 kb]
(414 Downloads)
| Abstract (HTML) (1312 Views)
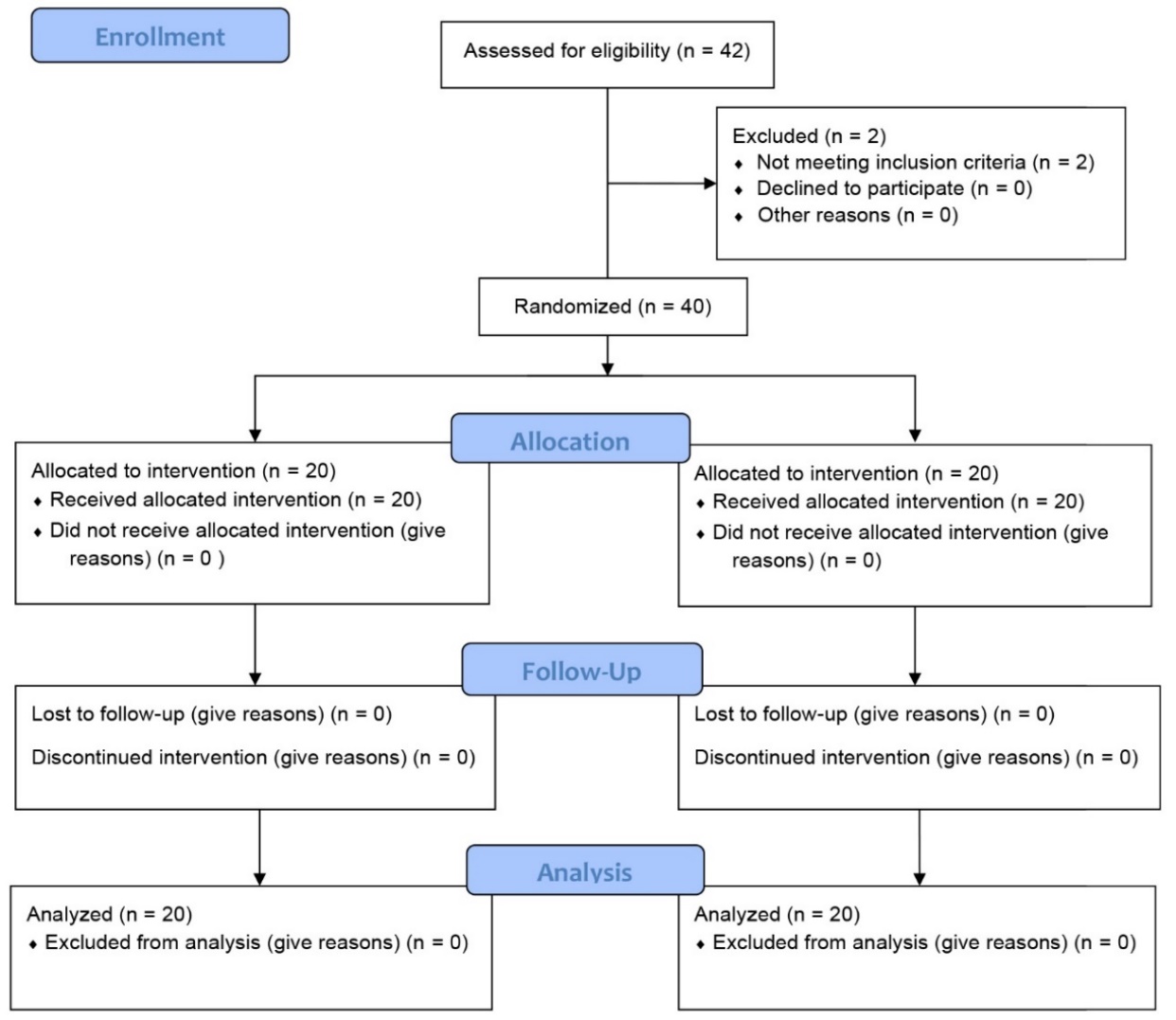
Table 2. Comparison of mean systolic blood pressure in the two studied groups at different times
Table 3. Comparison of mean diastolic blood pressure in the two studied groups at different times
Table 4. Comparison of average heart rate in the two studied groups at different times
Full-Text: (314 Views)
Abstract
Introduction: Maintaining hemodynamic stability during cataract surgery is crucial, particularly in elderly patients or those with underlying medical conditions. Melatonin and midazolam are among the medications used for sedation and improving intraoperative conditions; however, they may have different effects on hemodynamic parameters. This study aimed to compare the impact of these two medications on hemodynamic status before, during, and after cataract surgery.
Methods: This clinical trial was conducted on 40 patients scheduled for cataract surgery under general anesthesia. Participants were randomly assigned to one of two intervention groups; one of which received 0.1 mg/kg of oral melatonin, while the other received 70–80 µg/kg of intravenous midazolam. Both administrations occurred 1 h before surgery. A Saadat monitor was used to record hemodynamic parameters, namely systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR), at three intervals: 30 min before the operation, during the operation, and 6 h after the operation. Statistical analysis was performed in SPSS software (version 26), employing a significance threshold of p < 0.05.
Results: Analysis indicated that hemodynamic parameters, including SBP, DBP, and HR, were comparable between the two groups before, during, and after the operation, with no statistically significant intergroup differences (p > 0.05). In contrast, a significant intragroup change was observed in the melatonin group regarding HR over time (p = 0.005).
Conclusion: Although both medications were effective in maintaining hemodynamic stability, melatonin resulted in better stability of HR after surgery, compared to midazolam. Therefore, given its fewer side effects and efficacy on regulating HR, melatonin could be considered a safer alternative for patients prone to tachycardia in cataract surgery.
Key words: Cataract, General Anesthesia, Melatonin, Midazolam, Surgery
Introduction: Maintaining hemodynamic stability during cataract surgery is crucial, particularly in elderly patients or those with underlying medical conditions. Melatonin and midazolam are among the medications used for sedation and improving intraoperative conditions; however, they may have different effects on hemodynamic parameters. This study aimed to compare the impact of these two medications on hemodynamic status before, during, and after cataract surgery.
Methods: This clinical trial was conducted on 40 patients scheduled for cataract surgery under general anesthesia. Participants were randomly assigned to one of two intervention groups; one of which received 0.1 mg/kg of oral melatonin, while the other received 70–80 µg/kg of intravenous midazolam. Both administrations occurred 1 h before surgery. A Saadat monitor was used to record hemodynamic parameters, namely systolic blood pressure (SBP), diastolic blood pressure (DBP), and heart rate (HR), at three intervals: 30 min before the operation, during the operation, and 6 h after the operation. Statistical analysis was performed in SPSS software (version 26), employing a significance threshold of p < 0.05.
Results: Analysis indicated that hemodynamic parameters, including SBP, DBP, and HR, were comparable between the two groups before, during, and after the operation, with no statistically significant intergroup differences (p > 0.05). In contrast, a significant intragroup change was observed in the melatonin group regarding HR over time (p = 0.005).
Conclusion: Although both medications were effective in maintaining hemodynamic stability, melatonin resulted in better stability of HR after surgery, compared to midazolam. Therefore, given its fewer side effects and efficacy on regulating HR, melatonin could be considered a safer alternative for patients prone to tachycardia in cataract surgery.
Key words: Cataract, General Anesthesia, Melatonin, Midazolam, Surgery
Introduction
Cataract is a leading cause of visual impairment worldwide and in the United States, accounting for approximately 51% of blindness cases across the globe. Annually, millions of people worldwide undergo cataract surgery, a number that increases with the aging population (1). Some studies have indicated that in the near future, approximately 40 million people globally, particularly in developing countries, will be affected by cataract (2). Currently, surgery is the major method for treating and curing cataract, where the opaque and clouded lens is replaced with a clear artificial lens. Patients with risk factors, such as coronary artery disease or ischemic heart disease, advanced age, atherosclerosis, hypertension, and diabetes, are associated with a higher incidence of cardiac ischemic events during general anesthesia (3). Today, the field of anesthesiology operates to create the optimal conditions and minimal impairments for performing surgery, which is achieved through a state of deep sleep, adequate analgesia, and muscle relaxation (4).
The main goal of sedation in surgery is to ensure that the patient is calm during the injection and the procedure (5). Several medications, such as propofol and benzodiazepines (midazolam), are used for intraoperative sedation; however, due to their high effectiveness, they can cause poor patient cooperation before surgery (6). Some studies have proposed melatonin as a novel agent for pre-operative sedation in cataract surgery
(7-9). Melatonin, also known as N-acetyl-5-methoxytryptamine, is a neurohormone produced by the pineal gland; however, the results of numerous studies on this medication are controversial. Some studies have found that this medication, when used as a pre-anesthetic, induces sedation and stabilizes the overall physiological state before surgery without causing cognitive impairments, such as memory and recall deficits (10–12).
Maintenance of hemodynamic stability during surgery, particularly in cataract surgery, is of critical importance for several reasons (13). First, the population undergoing cataract surgery predominantly consists of elderly people, many of whom have underlying conditions, such as cardiovascular disease, hypertension, or diabetes (14). These patients are at a higher risk of blood pressure fluctuations and consequent impairments in tissue perfusion. Second, although cataract surgery is considered a minimally invasive procedure, the stress induced by the surgery itself and the anesthetic agents can lead to significant alterations in hemodynamic parameters (15).
Sudden changes in blood pressure, especially in elderly patients, can have serious consequences. Hypertension may lead to bleeding at the surgical site, whereas hypotension (a decrease in blood pressure) can cause reduced coronary and cerebral perfusion, which increases the risk of myocardial ischemia and cerebrovascular events, respectively (16). Furthermore, fluctuations in heart rate (HR), particularly medication-induced bradycardia, may lead to dangerous complications in patients with pre-existing cardiac conduction disorders (17).
From a physiological perspective, maintaining hemodynamic balance is essential for providing adequate oxygen to tissues and the proper removal of metabolites. Any disturbance in this balance can lead to tissue hypoxia, metabolic acidosis, and impaired function of vital organs (15). From a clinical standpoint, appropriate hemodynamic stability not only enhances intraoperative safety but can also lead to faster postoperative recovery, reduced length of hospital stay, and increased patient satisfaction. Furthermore, reducing hemodynamic fluctuations may also decrease postoperative complications, such as anesthesia-induced nausea and vomiting.
All the above-mentioned factors emphasize the importance of precise control of hemodynamic status during cataract surgery (18). Given the importance of maintaining hemodynamic stability and considering that studies on the efficacy of melatonin and its comparison with midazolam are limited, the present study was conducted with the aim of comparing the effect of melatonin and midazolam on the hemodynamic status of patients before, during, and after cataract surgery under general anesthesia.
Methods
This study was approved by the esteemed Research and Technology Deputy of Birjand University of Medical Sciences (ethical code: IR.BUMS.REC.1400.324) and registered in the Iranian Registry of Clinical Trials (code: IRCT20190618043934N15). This randomized controlled clinical trial was conducted from 2021 to 2022 on 40 patients who were candidates for cataract surgery under general anesthesia at the operating room of the Razi Hospital in Birjand, Iran.
The inclusion criteria were classification as American Society of Anesthesiologists class 1 or 2 and provision of informed consent to participate. The exclusion criteria consisted of drug addiction, non-cooperation with the study executor, heart failure, uncontrolled hypertension, anticoagulant, antiepileptic, immunosuppressive medication use, history of hepatic or renal disease, confusion, dementia, incapacity to communicate verbally, long-term narcotic use, barbiturate or antipsychotic medication treatments, allergies, and a body mass index below 18.5 or above 30.
The sample size was calculated based on the study performed by Patel et al. (2015) with 95% confidence and 80% power, resulting in 17 participants per group. Accounting for a potential 20% dropout rate, a total of 20 participants per group were considered.
Cataract is a leading cause of visual impairment worldwide and in the United States, accounting for approximately 51% of blindness cases across the globe. Annually, millions of people worldwide undergo cataract surgery, a number that increases with the aging population (1). Some studies have indicated that in the near future, approximately 40 million people globally, particularly in developing countries, will be affected by cataract (2). Currently, surgery is the major method for treating and curing cataract, where the opaque and clouded lens is replaced with a clear artificial lens. Patients with risk factors, such as coronary artery disease or ischemic heart disease, advanced age, atherosclerosis, hypertension, and diabetes, are associated with a higher incidence of cardiac ischemic events during general anesthesia (3). Today, the field of anesthesiology operates to create the optimal conditions and minimal impairments for performing surgery, which is achieved through a state of deep sleep, adequate analgesia, and muscle relaxation (4).
The main goal of sedation in surgery is to ensure that the patient is calm during the injection and the procedure (5). Several medications, such as propofol and benzodiazepines (midazolam), are used for intraoperative sedation; however, due to their high effectiveness, they can cause poor patient cooperation before surgery (6). Some studies have proposed melatonin as a novel agent for pre-operative sedation in cataract surgery
(7-9). Melatonin, also known as N-acetyl-5-methoxytryptamine, is a neurohormone produced by the pineal gland; however, the results of numerous studies on this medication are controversial. Some studies have found that this medication, when used as a pre-anesthetic, induces sedation and stabilizes the overall physiological state before surgery without causing cognitive impairments, such as memory and recall deficits (10–12).
Maintenance of hemodynamic stability during surgery, particularly in cataract surgery, is of critical importance for several reasons (13). First, the population undergoing cataract surgery predominantly consists of elderly people, many of whom have underlying conditions, such as cardiovascular disease, hypertension, or diabetes (14). These patients are at a higher risk of blood pressure fluctuations and consequent impairments in tissue perfusion. Second, although cataract surgery is considered a minimally invasive procedure, the stress induced by the surgery itself and the anesthetic agents can lead to significant alterations in hemodynamic parameters (15).
Sudden changes in blood pressure, especially in elderly patients, can have serious consequences. Hypertension may lead to bleeding at the surgical site, whereas hypotension (a decrease in blood pressure) can cause reduced coronary and cerebral perfusion, which increases the risk of myocardial ischemia and cerebrovascular events, respectively (16). Furthermore, fluctuations in heart rate (HR), particularly medication-induced bradycardia, may lead to dangerous complications in patients with pre-existing cardiac conduction disorders (17).
From a physiological perspective, maintaining hemodynamic balance is essential for providing adequate oxygen to tissues and the proper removal of metabolites. Any disturbance in this balance can lead to tissue hypoxia, metabolic acidosis, and impaired function of vital organs (15). From a clinical standpoint, appropriate hemodynamic stability not only enhances intraoperative safety but can also lead to faster postoperative recovery, reduced length of hospital stay, and increased patient satisfaction. Furthermore, reducing hemodynamic fluctuations may also decrease postoperative complications, such as anesthesia-induced nausea and vomiting.
All the above-mentioned factors emphasize the importance of precise control of hemodynamic status during cataract surgery (18). Given the importance of maintaining hemodynamic stability and considering that studies on the efficacy of melatonin and its comparison with midazolam are limited, the present study was conducted with the aim of comparing the effect of melatonin and midazolam on the hemodynamic status of patients before, during, and after cataract surgery under general anesthesia.
Methods
This study was approved by the esteemed Research and Technology Deputy of Birjand University of Medical Sciences (ethical code: IR.BUMS.REC.1400.324) and registered in the Iranian Registry of Clinical Trials (code: IRCT20190618043934N15). This randomized controlled clinical trial was conducted from 2021 to 2022 on 40 patients who were candidates for cataract surgery under general anesthesia at the operating room of the Razi Hospital in Birjand, Iran.
The inclusion criteria were classification as American Society of Anesthesiologists class 1 or 2 and provision of informed consent to participate. The exclusion criteria consisted of drug addiction, non-cooperation with the study executor, heart failure, uncontrolled hypertension, anticoagulant, antiepileptic, immunosuppressive medication use, history of hepatic or renal disease, confusion, dementia, incapacity to communicate verbally, long-term narcotic use, barbiturate or antipsychotic medication treatments, allergies, and a body mass index below 18.5 or above 30.
The sample size was calculated based on the study performed by Patel et al. (2015) with 95% confidence and 80% power, resulting in 17 participants per group. Accounting for a potential 20% dropout rate, a total of 20 participants per group were considered.
A convenience sampling method was employed to select patients who met the inclusion criteria. Subsequently, the patients were randomly allocated into two groups using simple randomization via the Random Allocation software (Figure 1). The first group received a melatonin tablet (0.1 mg/kg melatonin, manufactured by Razak Iran Company) 1 h before the surgery, while the second group received midazolam (at a dose of 70 µg/kg to 80 µg/kg intravenously) 1 h before the surgery. The patients were unaware of their group assignment (the patients were blinded).
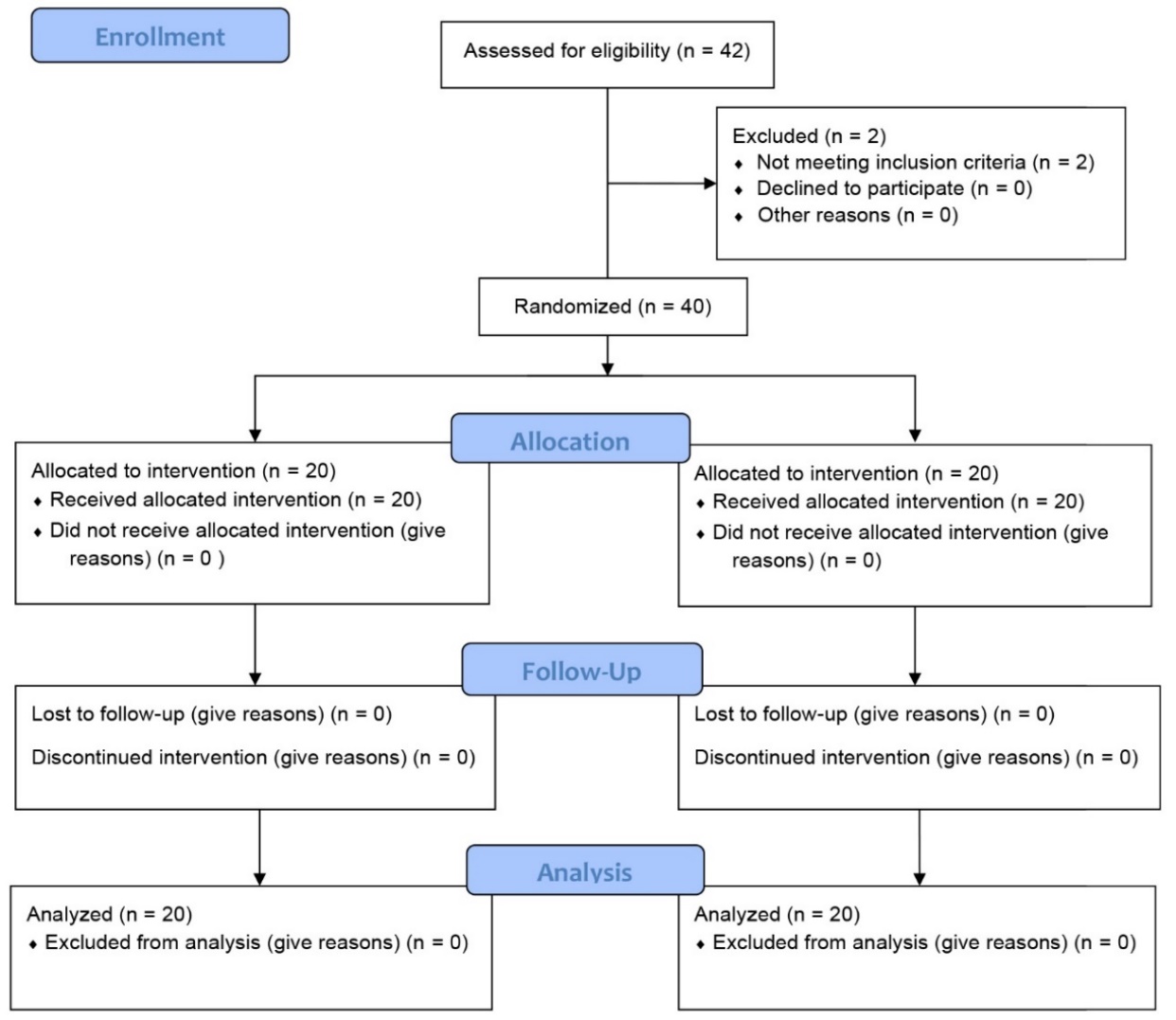
Figure 1. Flow chart of the study
Demographic information, including age, gender, educational level, place of residence, and the hemodynamic status of the patients before, during, and after the surgery, was recorded from the Saadat monitoring device by the study executor.
All patients underwent anesthesia induction with fentanyl (1 µg/kg), propofol (2 mg/kg), and atracurium (0.5 mg/kg). The surgical procedure for all patients was performed by a single surgeon. One hour before the surgery, the melatonin group received the melatonin tablet orally, and the midazolam group received the medication intravenously according to their body weight. Subsequently, the hemodynamic status of the patients (systolic blood pressure [SBP], diastolic blood pressure [DBP], and HR) was measured in both groups at 30 min before the surgery, during the surgery, and 6 h after the surgery. Both the patients and the researcher (assessor) were unaware of the group assignment and the administered medication (the study was double-blind).
Informed consent was obtained from all patients participating in the study. The hemodynamic assessment (SBP, DBP, and HR) of the patients before the surgery, during the surgery, and 6 h after the surgery was measured in both groups by the assessor and recorded on an anonymous checklist, which was designed based on the study objectives, by the study assessor.
After collection, the data were entered into SPSS software (version 26). Descriptive data were reported using mean and standard deviation, and relative frequency. For data analysis across the different groups, if the data had a normal distribution, an independent t-test and a paired t-test were used. If the data did not have a normal distribution, the Mann-Whitney U test, Chi-square test, or Fisher's exact test was employed at a significance level of α ≥ 0.05.
Results
Distribution of gender, education level, place of residence, and the mean age of the patients showed no significant difference between the two groups (p > 0.05) (table 1).
The mean SBP showed no significant difference between the midazolam and melatonin groups at the following time points: 30 min before surgery
(p = 0.738), during surgery (p = 0.799), and 6 h after surgery (p = 0.174). Furthermore, within each group, the mean SBP did not show a significant difference across the different time points in either the midazolam group (p = 0.948) or the melatonin group (p = 0.161) (table 2).
All patients underwent anesthesia induction with fentanyl (1 µg/kg), propofol (2 mg/kg), and atracurium (0.5 mg/kg). The surgical procedure for all patients was performed by a single surgeon. One hour before the surgery, the melatonin group received the melatonin tablet orally, and the midazolam group received the medication intravenously according to their body weight. Subsequently, the hemodynamic status of the patients (systolic blood pressure [SBP], diastolic blood pressure [DBP], and HR) was measured in both groups at 30 min before the surgery, during the surgery, and 6 h after the surgery. Both the patients and the researcher (assessor) were unaware of the group assignment and the administered medication (the study was double-blind).
Informed consent was obtained from all patients participating in the study. The hemodynamic assessment (SBP, DBP, and HR) of the patients before the surgery, during the surgery, and 6 h after the surgery was measured in both groups by the assessor and recorded on an anonymous checklist, which was designed based on the study objectives, by the study assessor.
After collection, the data were entered into SPSS software (version 26). Descriptive data were reported using mean and standard deviation, and relative frequency. For data analysis across the different groups, if the data had a normal distribution, an independent t-test and a paired t-test were used. If the data did not have a normal distribution, the Mann-Whitney U test, Chi-square test, or Fisher's exact test was employed at a significance level of α ≥ 0.05.
Results
Distribution of gender, education level, place of residence, and the mean age of the patients showed no significant difference between the two groups (p > 0.05) (table 1).
The mean SBP showed no significant difference between the midazolam and melatonin groups at the following time points: 30 min before surgery
(p = 0.738), during surgery (p = 0.799), and 6 h after surgery (p = 0.174). Furthermore, within each group, the mean SBP did not show a significant difference across the different time points in either the midazolam group (p = 0.948) or the melatonin group (p = 0.161) (table 2).
Table 1. Comparison of frequency distribution of gender, place of residence, and education level between the two midazolam and melatonin groups
| Parameter | Status | Midazolam N (%) |
Melatonin N (%) |
Chi-square test results | |
| Gender | Male | 10 (50) | 11 (55) | p = 1.000 | |
| Female | 10 (50) | 9 (45) | |||
| Place of Residence | City | 18 (90) | 18 (90) | p = 1.000 | |
| Village | 2 (10) | 2 (10) | |||
| Education Level | Illiterate and Primary | 12 (60) | 9 (45) | ||
| Middle School | 4 (20) | 5 (25) | p = 0.702 | ||
| High School and Diploma | 4 (20) | 6 (30) | |||
| Age | (Mean ± SD) | 61.5 ±9.4 | 63.5±12.3 | p = 0.743 | |
Table 2. Comparison of mean systolic blood pressure in the two studied groups at different times
| Systolic blood pressure | Midazolam | Melatonin | Mann-Whitney U Test Results |
| Mean ± SD | Mean ± SD | ||
| Median (Q1 – Q3) | Median (Q1 – Q3) | ||
| 30 minutes before surgery | 126 ± 16.02 127.5 (110 – 133) |
128 ± 16.12 128.5 (111.25 – 138.25) |
p = 0.738 |
| During surgery | 126.5 ± 18.45 125 (115 – 139.5) |
121.15 ± 30.37 120 (112.75 – 140) |
p = 0.799 |
| Six hours after surgery | 123.62 ± 9.26 125 (115 – 130) |
119.9 ± 9.13 117.5 (112.75 – 127.25) |
p = 0.174 |
| Friedman test results | p = 0.948 | p = 0.161 |
The mean DBP showed no significant difference between the midazolam and melatonin groups at 30 min before surgery (p = 0.718), during surgery (p = 0.157), and 6 h after surgery (p = 0.157). Furthermore, no significant differences were observed in the mean DBP across different time points within the midazolam group (p = 0.163) or the melatonin group (p = 0.642) (table 3).
Table 3. Comparison of mean diastolic blood pressure in the two studied groups at different times
| Diastolic blood pressure | Midazolam | Melatonin | Mann-Whitney U Test Results |
| Mean ± SD Median (Q1 – Q3) |
Mean ± SD Median (Q1 – Q3) |
||
| 30 minutes before surgery | 77.95 ± 8.68 77 (70 – 83.75) |
76.2 ± 5.74 77.5 (70 – 80) |
p = 0.718 |
| During surgery | 81.1 ± 8.17 80 (75.5 – 86.5) |
78.2 ± 13.4 76.5 (70.75 – 83.75) |
p = 0.157 |
| Six hours after surgery | 76.45 ± 7.41 75 (70.5 – 80.75) |
76 ± 7.01 76.5 (70.75 – 83.75) |
p = 0.157 |
| Friedman test results | p = 0.163 | p = 0.642 |
It should be noted that due to the non-normal distribution of some variables, the non-parametric Mann-Whitney U test was employed. The mean HR was not significantly different between the midazolam and melatonin groups at the following time points: 3o min before surgery
(p = 0.157), during surgery (p = 0.157), and 6 h after surgery (p = 0.081). Furthermore, within the midazolam group, the mean HR did not differ significantly across the various time points (p = 0.186). However, within the melatonin group, the mean HR did show a statistically significant difference across the different time points (p = 0.005) (table 4).
(p = 0.157), during surgery (p = 0.157), and 6 h after surgery (p = 0.081). Furthermore, within the midazolam group, the mean HR did not differ significantly across the various time points (p = 0.186). However, within the melatonin group, the mean HR did show a statistically significant difference across the different time points (p = 0.005) (table 4).
Table 4. Comparison of average heart rate in the two studied groups at different times
| Heart rate | Midazolam | Melatonin | Mann-Whitney Test Results |
| Mean ± SD Median (Q1 – Q3) |
Mean ± SD Median (Q1 – Q3) |
||
| 30 minutes before surgery | 77.1 ± 6.46 76.5 (71.25 – 80.75) |
70.2 ± 17.69* 72.5 (68 – 82.75) |
p = 0.157 |
| During surgery | 77.5 ± 9.59 79 (68.25 – 85.75) |
73 ± 10.3** 74.5 (62.75 – 79.75) |
p = 0.157 |
| 6 hours after surgery | 74.65 ± 10.47 75 (67.75 – 84.5) |
68.65 ± 10.7 68.5 (58.25 – 75.75) |
p = 0.081 |
| Friedman test results | p = 0.186 | p = 0.005 |
*Significant difference with 6 h after surgery (p = 0.043)
**Significant difference with 6 h after surgery (p = 0.008)
Discussion**Significant difference with 6 h after surgery (p = 0.008)
According to the findings, the melatonin and midazolam groups did not differ significantly in terms of age, gender, place of residence, or educational attainment (p > 0.05). A more reliable comparison of the pharmacological effects was made possible by the homogeneity of the groups. No significant difference was observed between the midazolam and melatonin groups in terms of the mean SBP 30 min before surgery, throughout surgery, and 6 h after the surgery. Additionally, the mean systolic and DBPs of the melatonin and midazolam groups did not differ significantly at different time points. Consistent with the current investigation, a study performed by Fassoulaki et al. found no significant difference in mean systolic and DBP between the melatonin and midazolam groups (19). Their study also revealed a significant drop in HR among melatonin users after surgery (p = 0.005), suggesting another potential advantage for maintaining stable hemodynamics. This finding on blood pressure alignment was supported by Haddadi et al., who also reported no significant intergroup differences in systolic and diastolic measures (20).
The findings suggested no significant differences between the impacts of the two medications on systolic or DBP across all perioperative stages (p > 0.05). This observation was consistent with those of a previous study carried out by Pechanova et al., demonstrating that melatonin does not exert a significant effect on blood pressure during cataract surgery (21).
With respect to HR, intergroup analysis showed no significant discrepancy at any measured interval (p > 0.05). However, a significant alteration in HR was observed within the melatonin group itself (p = 0.005), pointing to its potential modulatory influence. This finding was partially corroborated by a study performed by Kadhim Alkidsawi et al., which indicated that melatonin administration results in reduced HR fluctuations (22).
No significant difference in mean HR was observed between the midazolam and melatonin groups at any measured interval (30 minutes before the operation, during the operation, and 6 h after the operation). However, a significant variation in HR across these time points was found within the melatonin group, but not within the midazolam group.
This finding contrasts with those of a study conducted by Marzban et al., which reported a more pronounced reduction in HR with midazolam (23). This discrepancy may be attributed to differences in the timing of assessments and the dosage of melatonin (6 mg) used. However, results of the present study are consistent with those of a study performed by Haddadi et al. (20), Ismail et al., and Mowafi et al. (8, 24), all of whom found no significant intergroup difference in mean HR.
A notable point in this study was the greater stability of hemodynamic parameters in the melatonin group. Although no statistically significant difference in blood pressure was observed between the two groups, the trend of changes appeared more stable in the melatonin group. This finding could be important given that the patients undergoing cataract surgery are predominantly elderly, and hemodynamic fluctuations pose an increased risk for this high-risk group. A study performed by Baker et al. also demonstrated that melatonin causes fewer changes in mean arterial blood pressure (25).
Limitations of this study included convenience sampling, a relatively small sample size, and its single-center nature due to executive obstacles and practical constraints. Furthermore, the patient follow-up period was limited to 6 h post-operation, which may not be sufficient for a complete assessment of the effects of medications.
Conclusions
An examination of hemodynamic parameters before, during, and after surgery revealed that none of the aforementioned medications had any adverse effects on the vital signs of patients, and no serious hemodynamic instability requiring immediate medical intervention was observed.
Results of the present study indicated that melatonin may provide a more stable hemodynamic profile, compared to midazolam, as evidenced by a significant within-group reduction in HR variability. However, the absence of statistically significant intergroup differences precludes definitive claims of superiority. Confirming these outcomes requires further studies with expanded cohorts and extended follow-up.
The findings suggested no significant differences between the impacts of the two medications on systolic or DBP across all perioperative stages (p > 0.05). This observation was consistent with those of a previous study carried out by Pechanova et al., demonstrating that melatonin does not exert a significant effect on blood pressure during cataract surgery (21).
With respect to HR, intergroup analysis showed no significant discrepancy at any measured interval (p > 0.05). However, a significant alteration in HR was observed within the melatonin group itself (p = 0.005), pointing to its potential modulatory influence. This finding was partially corroborated by a study performed by Kadhim Alkidsawi et al., which indicated that melatonin administration results in reduced HR fluctuations (22).
No significant difference in mean HR was observed between the midazolam and melatonin groups at any measured interval (30 minutes before the operation, during the operation, and 6 h after the operation). However, a significant variation in HR across these time points was found within the melatonin group, but not within the midazolam group.
This finding contrasts with those of a study conducted by Marzban et al., which reported a more pronounced reduction in HR with midazolam (23). This discrepancy may be attributed to differences in the timing of assessments and the dosage of melatonin (6 mg) used. However, results of the present study are consistent with those of a study performed by Haddadi et al. (20), Ismail et al., and Mowafi et al. (8, 24), all of whom found no significant intergroup difference in mean HR.
A notable point in this study was the greater stability of hemodynamic parameters in the melatonin group. Although no statistically significant difference in blood pressure was observed between the two groups, the trend of changes appeared more stable in the melatonin group. This finding could be important given that the patients undergoing cataract surgery are predominantly elderly, and hemodynamic fluctuations pose an increased risk for this high-risk group. A study performed by Baker et al. also demonstrated that melatonin causes fewer changes in mean arterial blood pressure (25).
Limitations of this study included convenience sampling, a relatively small sample size, and its single-center nature due to executive obstacles and practical constraints. Furthermore, the patient follow-up period was limited to 6 h post-operation, which may not be sufficient for a complete assessment of the effects of medications.
Conclusions
An examination of hemodynamic parameters before, during, and after surgery revealed that none of the aforementioned medications had any adverse effects on the vital signs of patients, and no serious hemodynamic instability requiring immediate medical intervention was observed.
Results of the present study indicated that melatonin may provide a more stable hemodynamic profile, compared to midazolam, as evidenced by a significant within-group reduction in HR variability. However, the absence of statistically significant intergroup differences precludes definitive claims of superiority. Confirming these outcomes requires further studies with expanded cohorts and extended follow-up.
Acknowledgments
The writers would like to express their deepest gratitude to the esteemed study participants whose patience and cooperation made this research possible. They also would like to sincerely thank the respected colleagues at Razi Hospital and Birjand University of Medical Sciences, who assisted in data collection and project execution.
Funding
This article was derived from a medical thesis (code: 456421) approved by Birjand University of Medical Sciences, Birjand, Iran.
Conflict of Interest
There are no conflicts of interest associated with this publication, and the authors have no financial or other interests that could affect the objectivity of this research.
could be considered a safer alternative for patients prone to tachycardia in cataract surgery.Funding
This article was derived from a medical thesis (code: 456421) approved by Birjand University of Medical Sciences, Birjand, Iran.
Conflict of Interest
There are no conflicts of interest associated with this publication, and the authors have no financial or other interests that could affect the objectivity of this research.
Type of Study: Research |
Subject:
Ophthalmology
Received: 2025/06/7 | Accepted: 2025/08/13 | ePublished ahead of print: 2025/09/7 | Published: 2025/09/18
Received: 2025/06/7 | Accepted: 2025/08/13 | ePublished ahead of print: 2025/09/7 | Published: 2025/09/18
References
1. Pascolini D, Mariotti SP. Global estimates of visual impairment: 2010. Br J Ophthalmol. 2012;96(5):614-8. [DOI:10.1136/bjophthalmol-2011-300539]
2. Flessa S. Cataract surgery in low-income countries: a good deal! . Healthcare (Basel). 2022; 10:2580. [DOI:10.3390/healthcare10122580]
3. Han X, Zhang J, Liu Z, Tan X, Jin G, He M, et al. Real-world visual outcomes of cataract surgery based on population-based studies: a systematic review. Br J Ophthalmol. 2023;107(8):1056-65. [DOI:10.1136/bjophthalmol-2021-320997]
4. Lersch F, Eke T. Anaesthesia for cataract surgery. Cataract and Lens Surgery: Springer; 2023. p. 143-58. [DOI:10.1007/978-3-031-05394-8_22]
5. Sanatkar M, Goudarzi M, Espahbodi E. Comparison of the efficacy of two pre-treatment medications of dexmedetomidine-fentanyl and midazolam-fentanyl in cataract surgery. Tehran Univ Med J. 2020;78(3):155-64.
6. Perumal D, Dudley RA, Gan S, Boscardin WJ, Gill A, Gelb AW, et al. Anesthesia care for cataract surgery in Medicare beneficiaries. JAMA Intern Med. 2022;182(11):1171-80. [DOI:10.1001/jamainternmed.2022.4333]
7. Hosni K, Mighri F, Knani L, Mahjoub A, Nouri H, Benjazia K. Efficacy of a premedication with melatonin during cataract surgery under peribulbar block: Study protocol for a prospective randomized double-blinded study. Tunis Med. 2022;100(10):713-18.
8. Ismail SA, Mowafi HA. Melatonin provides anxiolysis, enhances analgesia, decreases intraocular pressure, and promotes better operating conditions during cataract surgery under topical anesthesia. Anesth Analg. 2009;108(4):1146-51. [DOI:10.1213/ane.0b013e3181907ebe]
9. Malekshoar M, Tahmoresi N, Adibi P, Zarei T, Vatankhah M. Investigating the effect of melatonin and tizanidine on hemodynamic parameters and anxiety in patients undergoing cataract surgery: A double-blind randomized clinical trial study. Pars J Med Sci. 2023;21(4):18-25.
10. Khezri MB, Merate H. The effects of melatonin on anxiety and pain scores of patients, intraocular pressure, and operating conditions during cataract surgery under topical anesthesia. Indian J Ophthalmol. 2013;61(7):319-24. [DOI:10.4103/0301-4738.99637]
11. Mahmoudi H, Ebadi A, Salimi SH, Najafi Mehri S, Mokhtari Noori J, Shokrollahi F. Effect of nurse communication with patients on anxiety, depression, and stress level of emergency ward patients. J Crit Care Nurs. 2010;3(1):3-4.
12. Patel T, Kurdi MS. A comparative study between oral melatonin and oral midazolam on preoperative anxiety, cognitive, and psychomotor functions. J Anaesthesiol Clin Pharmacol. 2015;31(1):37-43. [DOI:10.4103/0970-9185.150534]
13. Khademi S, Jouybar R, Ahmadi S, Asmarian N, Ghadimi M, Salari M, et al. Hemodynamic Changes after Continuing or Omitting Regular Angiotensin Converting Enzyme Inhibitors before Cataract Surgery: A Comparative Study. Curr Hypertens Rev. 2023;19(1):59-65. [DOI:10.2174/1573402119666230112110328]
14. Yang L, Li H, Zhao X, Pan Y. Association between cataract surgery and age‐related macular degeneration: a systematic review and meta‐analysis. J Ophthalmol. 2022;2022(1):6780901. [DOI:10.1155/2022/6780901]
15. Zavgorodnia N, Mykhailenko N, Bezugly M, Poplavska I. Effects of phacoemulsification cataract surgery on hydro-and hemodynamics in highly myopic eyes. Bull Probl Biol Med. 2021;159(1):62-6. [DOI:10.29254/2077-4214-2021-1-159-62-66]
16. Hari TS, Sudha TS, Varghese AM, Sasanka KK, Thangaraju P. A study of risk factors and complications in elderly hypertensive subjects. J Family Med Prim Care. 2021;10(6):2230-4. [DOI:10.4103/jfmpc.jfmpc_1959_20]
17. Ono T, Iwasaki T, Kawahara K, Agune Y, Mori Y, Nejima R, et al. Early intervention for perioperative hypertension in cataract surgery. Graefes Arch Clin Exp Ophthalmol. 2023;261(1):147-54. [DOI:10.1007/s00417-022-05815-2]
18. Nazari M, Akbari F, Dehghani A. Comparing the effects of remifentanil with fentanyl on pain intensity, hemodynamic status and post-anesthesia complications of cataract surgery candidates. Medicinal, Psychological, and Health Research Journal . 2025;1(4):116-25.
19. Fassoulaki A, Triga A, Melemeni A, Sarantopoulos C. Multimodal analgesia with gabapentin and local anesthetics prevents acute and chronic pain after breast surgery for cancer. Anesth Analg. 2005;101(5):1427-32. [DOI:10.1213/01.ANE.0000180200.11626.8E]
20. Haddadi S, Shahrokhirad R, Ansar MM, Marzban S, Akbari M, Parvizi A. Efficacy of Preoperative Administration of Acetaminophen and Melatonin on Retrobulbar Block Associated Pain in Cataract Surgery. Aapm. 2018;8(5):39-43. [DOI:10.5812/aapm.61041]
21. Pechanova O, Paulis L, Simko F. Peripheral and central effects of melatonin on blood pressure regulation. Int J Mol Sci. 2014;15(10):17920-37. [DOI:10.3390/ijms151017920]
22. Kadhim Alkidsawi MJ, Hussein HA, Alhamaidah MF, Mahdi AH, Kahloul M. Investigating the Influence of Melatonin on the Respiratory Rate, Heart Rate, and Oxygen Saturation in Paediatric Surgical Care: A Randomized Double-Blinding Trial. Pak J Life Soc Sci. 2024;22(1):2065. [DOI:10.57239/PJLSS-2024-22.1.00151]
23. marzban s, haddadi s, taheri fard p, atrkar roshan z, parvizi a, panjtan panah m. Comparison of the effect of Melatonin and Gabapentin on pain and anxiety in patients undergoing cataract surgery with Phacoemulsification with topical anesthesia. Anesthesiology and Pain. 2016;7(3):1-10.
24. Mowafi HA, Ismail SA. Melatonin improves tourniquet tolerance and enhances postoperative analgesia in patients receiving intravenous regional anesthesia. Anesthesia & Analgesia. 2008;107(4):1422-6. [DOI:10.1213/ane.0b013e318181f689]
25. Baker J, Kimpinski K. Role of melatonin in blood pressure regulation: An adjunct anti‐hypertensive agent. Clin Exp Pharmacol Physiol. 2018;45(8):755-66. [DOI:10.1111/1440-1681.12942]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |