Volume 13, Issue 4 (10-2025)
J Surg Trauma 2025, 13(4): 164-166 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Amouzeshi A, Shahriary E, Sabaghi Qalanou M, Shakhs Emempour F, Hosseini Zargaz S E, Ghadimi M et al . A Case Report of a COVID-19-Positive Patient Undergoing Emergency Coronary Artery Bypass Grafting Surgery: A Novel Experience. J Surg Trauma 2025; 13 (4) :164-166
URL: http://jsurgery.bums.ac.ir/article-1-485-en.html
URL: http://jsurgery.bums.ac.ir/article-1-485-en.html
Ahmad Amouzeshi 

 , Ensieh Shahriary
, Ensieh Shahriary 
 , Motahareh Sabaghi Qalanou
, Motahareh Sabaghi Qalanou 
 , Fatemeh Shakhs Emempour
, Fatemeh Shakhs Emempour 

 , Seyyed Ebrahim Hosseini Zargaz
, Seyyed Ebrahim Hosseini Zargaz 

 , Maryam Ghadimi
, Maryam Ghadimi 

 , Mahmoud Ganjifard *
, Mahmoud Ganjifard * 




 , Ensieh Shahriary
, Ensieh Shahriary 
 , Motahareh Sabaghi Qalanou
, Motahareh Sabaghi Qalanou 
 , Fatemeh Shakhs Emempour
, Fatemeh Shakhs Emempour 

 , Seyyed Ebrahim Hosseini Zargaz
, Seyyed Ebrahim Hosseini Zargaz 

 , Maryam Ghadimi
, Maryam Ghadimi 

 , Mahmoud Ganjifard *
, Mahmoud Ganjifard * 


Department of Anesthesiology, Faculty of Medicine, Birjand University of Medical Sciences, Birjand, Iran
Full-Text [PDF 368 kb]
(383 Downloads)
| Abstract (HTML) (1316 Views)
Discussion
Performing surgery on patients with COVID-19 is often unavoidable, depending on their clinical condition, acuity, and emergency status. Underlying COVID pathologies that have significantly increased intra- and postoperative complications can include inflammatory response, cardiovascular and respiratory disorders, and coagulation abnormalities (6). Numerous studies to date have recommended postponing CABG surgery whenever possible due to the potential pulmonary complications that patients may experience postoperatively. A study by Barkhordari et al. investigated 25 patients (off‐pump cardiac surgery [n=4] and on‐pump cardiac surgery [21]) with COVID-19 undergoing cardiac surgery. The results indicated that while initial respiratory and pulmonary outcomes were satisfactory, there was a significant difference in ICU readmission rates between the COVID-19 and non-COVID-19 groups. It was also reported that the mean length of stay in the ICU was 1.8 days for the non-COVID-19 group and 3 days for the COVID-19 group. Moreover, the mortality rate was found to be 16% for the COVID-19 group and 2% for the other group, despite similar baseline characteristics. Ultimately, it was recommended that cardiac surgeries for COVID-19 patients who were candidates for surgery be postponed (7, 8). One of the complications of CPB is the activation of the inflammatory system, leading to pulmonary collapse and an increase in inflammatory factors within the lungs. Various studies have demonstrated that in patients undergoing cardiac surgery with pulmonary hypertension, simultaneous ventilation during CPB significantly reduces the incidence of atelectasis, pulmonary collapse, pulmonary hypertension, and pulmonary edema postoperatively due to the continued ventilation of the lungs. In a clinical trial involving 48 pediatric patients undergoing congenital cardiac surgery, patients were divided into three groups: Group 1 (with standard protective tidal volume), Group 2 (with continuous positive airway pressure), and Group 3 (with no mechanical ventilation). The results of this study revealed that mechanical ventilation during CABG in Groups 1 and 2 reduced the incidence of postoperative atelectasis by two-thirds and significantly mitigated the incidence of pulmonary complications (5). In another study, results demonstrated that patients who underwent CABG surgery during the COVID-19 pandemic had significantly higher pulmonary complications, including atelectasis and pulmonary edema, compared to the control group (6). The results of a separate study demonstrated a significantly higher prevalence of atelectasis in COVID-19-positive patients, and the mean length of stay in the ICU was also greater in patients with more extensive atelectasis. One factor that past studies have shown to increase length of stay in the ICU and the incidence of atelectasis is the absence of mechanical ventilation during CPB. Therefore, considering this issue and the higher incidence of atelectasis in COVID-19-positive patients, it appears that performing mechanical ventilation is effective in reducing both the length of stay in the ICU and the incidence of atelectasis (7). Finally, it is suggested that studies with larger sample sizes be conducted in this area to more thoroughly investigate this method.
Conclusions
Given the controversial results regarding surgery in COVID-19-positive patients, it seems that using mechanical ventilation during CPB can greatly reduce the exacerbation of pulmonary complications caused by this disease. It is recommended that a large-scale study be conducted in this regard in the future.
Conflict of Interest
The authors declare no conflict of interest regarding the publication of the study.
Full-Text: (271 Views)
Abstract
Coronary artery bypass graft (CABG) surgery with the help of cardiopulmonary bypass (CPB) can cause complications for the lungs after the operation. A 62-year-old woman was reported to have a positive COVID-19 test; however, due to her cardiac conditions, she was scheduled for an emergency CABG surgery. The patient was experiencing symptoms of chest pain and dyspnea, and her pulmonary artery systolic pressure was 45 mmHg. Considering that the patient would be undergoing surgery with CPB, a ventilation strategy was planned to reduce the risk of pulmonary complications during the procedure. The patient recovered well without any specific pulmonary complications after the surgery. It seems that patients with positive COVID-19 are at risk of pulmonary complications. Therefore, a ventilation strategy during the procedure can significantly reduce the risk of pulmonary complications and their consequences after the surgery.
Keywords: Complications, Coronary Artery Bypass, COVID-19, Surgery
Introduction
The coronavirus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is regarded as a serious global health crisis. Scientific reports have documented cases of cardiovascular involvement in addition to common pulmonary damage, demonstrating a complex interaction between the high replication capacity of SARS-CoV-2 and various clinical manifestations, which commonly culminate in an unfavorable prognosis [1]. Pulmonary damage and its complications are currently common following cardiac surgery. Factors contributing to the development and exacerbation of pulmonary complications encompass general anesthesia, pulmonary collapse (pulmonary collapse or atelectasis is defined as pulmonary collapse that occurs after anesthetic induction), and the activation of the inflammatory system. One effective method for mitigating postoperative pulmonary complications is the use of ventilation during CPB (2-4). The case we reported involved a patient with COVID-19 and pulmonary hypertension undergoing emergency CABG surgery.
Case
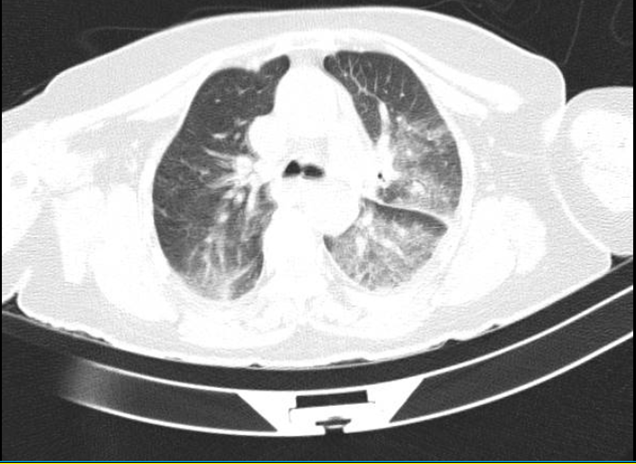
A 62-year-old woman (weighing 55 kg) was referred from another center due to cardiac arrest and ventricular fibrillation (VF). The patient had fever, myalgia, and cough. Since her SPO2 was 89%, she was intubated. The patient had a history of hypertension and diabetes. Angiographic investigation revealed three-vessel disease with an ejection fraction of 35%. The patient experienced severe chest pain and then underwent emergency CABG surgery. A computed tomography (CT) scan of the lungs showed ground-glass opacities in both lung fields, predominantly in the left lung. Additionally, consolidation opacity was observed in the left lower lobe. A calcified nodule measuring 7×9 mm was noted in the apex of the left lung (Figure 1). Laboratory tests revealed a C-reactive protein level of 60.4 (mg/dl). The patient also tested positive for both COVID-19 and influenza. Due to pulmonary hypertension (45mmHg) and the potential for exacerbated respiratory complications postoperatively, according to the study of Meng‑Qiu Zhang et al. (5), a positive end-expiratory pressure of 5 mmHg, a respiratory rate of 12, and a lung volume of 6 mL/kg, equivalent to 360 mL, were applied to the patient during CPB. Postoperatively, the patient was transferred from the intensive care unit (ICU) to the cardiology ward after two days, without developing any pulmonary collapse. The patient was then discharged from the hospital in good general condition after five days (SPO2=94%)
Coronary artery bypass graft (CABG) surgery with the help of cardiopulmonary bypass (CPB) can cause complications for the lungs after the operation. A 62-year-old woman was reported to have a positive COVID-19 test; however, due to her cardiac conditions, she was scheduled for an emergency CABG surgery. The patient was experiencing symptoms of chest pain and dyspnea, and her pulmonary artery systolic pressure was 45 mmHg. Considering that the patient would be undergoing surgery with CPB, a ventilation strategy was planned to reduce the risk of pulmonary complications during the procedure. The patient recovered well without any specific pulmonary complications after the surgery. It seems that patients with positive COVID-19 are at risk of pulmonary complications. Therefore, a ventilation strategy during the procedure can significantly reduce the risk of pulmonary complications and their consequences after the surgery.
Keywords: Complications, Coronary Artery Bypass, COVID-19, Surgery
Introduction
The coronavirus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is regarded as a serious global health crisis. Scientific reports have documented cases of cardiovascular involvement in addition to common pulmonary damage, demonstrating a complex interaction between the high replication capacity of SARS-CoV-2 and various clinical manifestations, which commonly culminate in an unfavorable prognosis [1]. Pulmonary damage and its complications are currently common following cardiac surgery. Factors contributing to the development and exacerbation of pulmonary complications encompass general anesthesia, pulmonary collapse (pulmonary collapse or atelectasis is defined as pulmonary collapse that occurs after anesthetic induction), and the activation of the inflammatory system. One effective method for mitigating postoperative pulmonary complications is the use of ventilation during CPB (2-4). The case we reported involved a patient with COVID-19 and pulmonary hypertension undergoing emergency CABG surgery.
Case
A 62-year-old woman (weighing 55 kg) was referred from another center due to cardiac arrest and ventricular fibrillation (VF). The patient had fever, myalgia, and cough. Since her SPO2 was 89%, she was intubated. The patient had a history of hypertension and diabetes. Angiographic investigation revealed three-vessel disease with an ejection fraction of 35%. The patient experienced severe chest pain and then underwent emergency CABG surgery. A computed tomography (CT) scan of the lungs showed ground-glass opacities in both lung fields, predominantly in the left lung. Additionally, consolidation opacity was observed in the left lower lobe. A calcified nodule measuring 7×9 mm was noted in the apex of the left lung (Figure 1). Laboratory tests revealed a C-reactive protein level of 60.4 (mg/dl). The patient also tested positive for both COVID-19 and influenza. Due to pulmonary hypertension (45mmHg) and the potential for exacerbated respiratory complications postoperatively, according to the study of Meng‑Qiu Zhang et al. (5), a positive end-expiratory pressure of 5 mmHg, a respiratory rate of 12, and a lung volume of 6 mL/kg, equivalent to 360 mL, were applied to the patient during CPB. Postoperatively, the patient was transferred from the intensive care unit (ICU) to the cardiology ward after two days, without developing any pulmonary collapse. The patient was then discharged from the hospital in good general condition after five days (SPO2=94%)
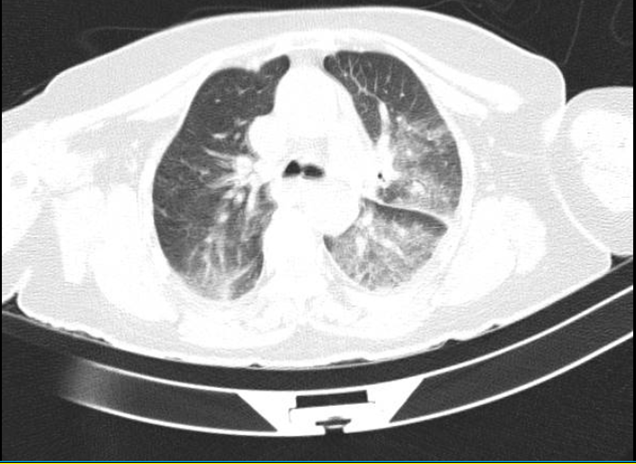
Figure1. A computed tomography scan of the lungs
Discussion
Performing surgery on patients with COVID-19 is often unavoidable, depending on their clinical condition, acuity, and emergency status. Underlying COVID pathologies that have significantly increased intra- and postoperative complications can include inflammatory response, cardiovascular and respiratory disorders, and coagulation abnormalities (6). Numerous studies to date have recommended postponing CABG surgery whenever possible due to the potential pulmonary complications that patients may experience postoperatively. A study by Barkhordari et al. investigated 25 patients (off‐pump cardiac surgery [n=4] and on‐pump cardiac surgery [21]) with COVID-19 undergoing cardiac surgery. The results indicated that while initial respiratory and pulmonary outcomes were satisfactory, there was a significant difference in ICU readmission rates between the COVID-19 and non-COVID-19 groups. It was also reported that the mean length of stay in the ICU was 1.8 days for the non-COVID-19 group and 3 days for the COVID-19 group. Moreover, the mortality rate was found to be 16% for the COVID-19 group and 2% for the other group, despite similar baseline characteristics. Ultimately, it was recommended that cardiac surgeries for COVID-19 patients who were candidates for surgery be postponed (7, 8). One of the complications of CPB is the activation of the inflammatory system, leading to pulmonary collapse and an increase in inflammatory factors within the lungs. Various studies have demonstrated that in patients undergoing cardiac surgery with pulmonary hypertension, simultaneous ventilation during CPB significantly reduces the incidence of atelectasis, pulmonary collapse, pulmonary hypertension, and pulmonary edema postoperatively due to the continued ventilation of the lungs. In a clinical trial involving 48 pediatric patients undergoing congenital cardiac surgery, patients were divided into three groups: Group 1 (with standard protective tidal volume), Group 2 (with continuous positive airway pressure), and Group 3 (with no mechanical ventilation). The results of this study revealed that mechanical ventilation during CABG in Groups 1 and 2 reduced the incidence of postoperative atelectasis by two-thirds and significantly mitigated the incidence of pulmonary complications (5). In another study, results demonstrated that patients who underwent CABG surgery during the COVID-19 pandemic had significantly higher pulmonary complications, including atelectasis and pulmonary edema, compared to the control group (6). The results of a separate study demonstrated a significantly higher prevalence of atelectasis in COVID-19-positive patients, and the mean length of stay in the ICU was also greater in patients with more extensive atelectasis. One factor that past studies have shown to increase length of stay in the ICU and the incidence of atelectasis is the absence of mechanical ventilation during CPB. Therefore, considering this issue and the higher incidence of atelectasis in COVID-19-positive patients, it appears that performing mechanical ventilation is effective in reducing both the length of stay in the ICU and the incidence of atelectasis (7). Finally, it is suggested that studies with larger sample sizes be conducted in this area to more thoroughly investigate this method.
Conclusions
Given the controversial results regarding surgery in COVID-19-positive patients, it seems that using mechanical ventilation during CPB can greatly reduce the exacerbation of pulmonary complications caused by this disease. It is recommended that a large-scale study be conducted in this regard in the future.
Conflict of Interest
The authors declare no conflict of interest regarding the publication of the study.
Type of Study: Case Report |
Subject:
General Surgery
Received: 2025/06/24 | Accepted: 2025/07/30 | ePublished ahead of print: 2025/08/16 | Published: 2025/10/14
Received: 2025/06/24 | Accepted: 2025/07/30 | ePublished ahead of print: 2025/08/16 | Published: 2025/10/14
References
1. Romiti S, Totaro M, Laderchi A, Peruzzi M, Vinciguerra M, Greco E. Case report: Emergency CABG following failure of PTCA in a COVID-19 patient. Front Cardiovasc Med. 2021;7: 620610. [DOI:10.3389/fcvm.2020.620610]
2. Ryz S, Menger J, Veraar C, Datler P, Mouhieddine M, Zingher F, et al. Identifying high-risk patients for severe pulmonary complications after Cardiosurgical Procedures as a Target Group for further Assessment of lung-protective strategies J Cardiothorac Vasc Anesth. 2024;38(2):445-50. [DOI:10.1053/j.jvca.2023.11.030]
3. Rogers CA, Mazza G, Maishman R, Thirard R, Evans J, De Jesus S, et al. Low Frequency Ventilation During Cardiopulmonary Bypass to Protect Postoperative Lung Function in Cardiac Valvular Surgery: The PROTECTION Phase II Randomized Trial. J Am Heart Assoc. 2024;13(19):e035011. [DOI:10.1161/JAHA.124.035011]
4. Malbouisson LM, Humberto F, Rodrigues RD, Carmona MJ, Auler Jr JO. Atelectasias durante anestesia: fisiopatologia e tratamento. Rev Bras Anestesiol. 2008;58(1):73-83. [DOI:10.1590/S0034-70942008000100011]
5. Zhang MQ, Liao YQ, Yu H, Li XF, Shi W, Jing WW, et al. Effect of ventilation strategy during cardiopulmonary bypass on postoperative pulmonary complications after cardiac surgery: a randomized clinical trial. J Cardiothorac Surg. 2021;16(1):1-8. [DOI:10.1186/s13019-021-01699-1]
6. Ayati A, Hosseini K, Hadizadeh A, Jalali A, Lotfi‐Tokaldany M, Milan N, et al. Surgical coronary revascularization in patients with COVID‐19; complications and outcomes: A retrospective cohort study. Health Sci Rep. 2022;5(5):e751. [DOI:10.1002/hsr2.751]
7. Gomes WJ, Rocco I, Pimentel WS, Pinheiro AH, Souza PM, Costa LA, et al. COVID-19 in the perioperative period of cardiovascular surgery: the Brazilian experience. Braz J Cardiovasc Surg. 2021;36(6):725-35. [DOI:10.21470/1678-9741-2021-0960]
8. Barkhordari K, Khajavi MR, Bagheri J, Nikkhah S, Shirzad M, Barkhordari S, et al. Early respiratory outcomes following cardiac surgery in patients with COVID‐19. J Card Surg 2020;35(10):2479-85. [DOI:10.1111/jocs.14915]
9. Magdy M, Elnegeery NA, El Rahamawy GA, Elgamal MA, Hayes SM. Evaluation of the effect of ventilation strategies during cardiopulmonary bypass on postoperative pulmonary complication in pediatric cardiac surgery: A randomized prospective study. Int J Health Sci. 2022;6(9),782-93. [DOI:10.53730/ijhs.v6nS9.12506]
10. Mingote Á, Albajar A, García Benedito P, Garcia-Suarez J, Pelosi P, Ball L, et al. Prevalence and clinical consequences of atelectasis in SARS-CoV-2 pneumonia: a computed tomography retrospective cohort study. BMC Pulm Med. 2021;21(1):267. [DOI:10.1186/s12890-021-01638-9]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |