Article in Press
Back to the articles list |
Back to browse issues page
Department of Emergency Medicine, Sina hospital, Tehran University of Medical Sciences, Tehran, Iran
Full-Text [PDF 400 kb]
(19 Downloads)
| Abstract (HTML) (34 Views)
Full-Text: (10 Views)
Abstract
Type A aortic dissection (TAAD) is a medical emergency that can lead to catastrophic complications, including malperfusion of vital organs and extremities. Popliteal artery embolism as a result of TAAD is rare but can result in acute limb ischemia, which carries a high risk of limb loss if not promptly addressed. This study aimed to present a case of a 72-year-old male with a history of hypertension and hyperlipidemia who presented to the emergency department with sudden-onset, severe chest pain radiating to his back and acute pain and coldness in his right lower extremity. Physical examination revealed a pale, cool, and pulseless right lower extremity with diminished sensation and motor function. Initial imaging, including transthoracic echocardiography and computed tomography angiography, confirmed TAAD with a thrombus occluding the right popliteal artery. In transthoracic echocardiography, the aortic valve appeared structurally normal with no evidence of regurgitation or stenosis. The patient underwent emergent surgical repair of the aortic dissection and thrombectomy of the popliteal artery, with successful revascularization and transfer to the intensive care unit postoperatively. This case highlighted the rare but critical complication of acute limb ischemia secondary to TAAD, emphasizing the importance of a high index of suspicion for aortic dissection in patients presenting with limb ischemia, particularly in the presence of risk factors. A multidisciplinary approach involving early imaging, prompt surgical intervention, and limb revascularization is crucial to improving outcomes. Despite advances in management, acute limb ischemia due to TAAD remains associated with high morbidity and mortality, underscoring the need for further research to optimize diagnostic and therapeutic strategies.
Key words: Aortic Dissection, Arterial Occlusive Diseases, Chest Pain, Emergency Medical Services
Type A aortic dissection (TAAD) is a medical emergency that can lead to catastrophic complications, including malperfusion of vital organs and extremities. Popliteal artery embolism as a result of TAAD is rare but can result in acute limb ischemia, which carries a high risk of limb loss if not promptly addressed. This study aimed to present a case of a 72-year-old male with a history of hypertension and hyperlipidemia who presented to the emergency department with sudden-onset, severe chest pain radiating to his back and acute pain and coldness in his right lower extremity. Physical examination revealed a pale, cool, and pulseless right lower extremity with diminished sensation and motor function. Initial imaging, including transthoracic echocardiography and computed tomography angiography, confirmed TAAD with a thrombus occluding the right popliteal artery. In transthoracic echocardiography, the aortic valve appeared structurally normal with no evidence of regurgitation or stenosis. The patient underwent emergent surgical repair of the aortic dissection and thrombectomy of the popliteal artery, with successful revascularization and transfer to the intensive care unit postoperatively. This case highlighted the rare but critical complication of acute limb ischemia secondary to TAAD, emphasizing the importance of a high index of suspicion for aortic dissection in patients presenting with limb ischemia, particularly in the presence of risk factors. A multidisciplinary approach involving early imaging, prompt surgical intervention, and limb revascularization is crucial to improving outcomes. Despite advances in management, acute limb ischemia due to TAAD remains associated with high morbidity and mortality, underscoring the need for further research to optimize diagnostic and therapeutic strategies.
Key words: Aortic Dissection, Arterial Occlusive Diseases, Chest Pain, Emergency Medical Services
Introduction
Popliteal artery embolism is an uncommon but critical complication of Type A aortic dissection (TAAD), a life-threatening condition that requires immediate intervention. While chest pain is the hallmark symptom of TAAD, the migration of intimal flaps or thrombi into peripheral arteries, such as the popliteal artery, can result in severe limb-threatening complications. This case report aimed to describe an elderly male with a history of hypertension and hyperlipidemia who presented with sudden-onset chest pain and acute ischemia of the right lower extremity due to popliteal artery embolism secondary to TAAD. The case underscored the diagnostic and therapeutic challenges associated with this rare presentation and highlighted the importance of considering TAAD in the differential diagnosis of acute limb ischemia (ALI), particularly in patients with cardiovascular risk factors. Early recognition, prompt imaging, and a multidisciplinary approach to management are essential to improve outcomes in this high-risk population (1,2).
Case
A 72-year-old male with a history of poorly controlled hypertension and hyperlipidemia presented to the Emergency Department with sudden-onset, severe chest pain radiating to his back. He also reported acute-onset pain and coldness in his right lower extremity. Physical examination revealed that he was tachycardic (heart rate: 110 bpm) and hypertensive (blood pressure: 160/100 mmHg). The right lower extremity was pale, cool, and pulseless, with diminished sensation and motor function.
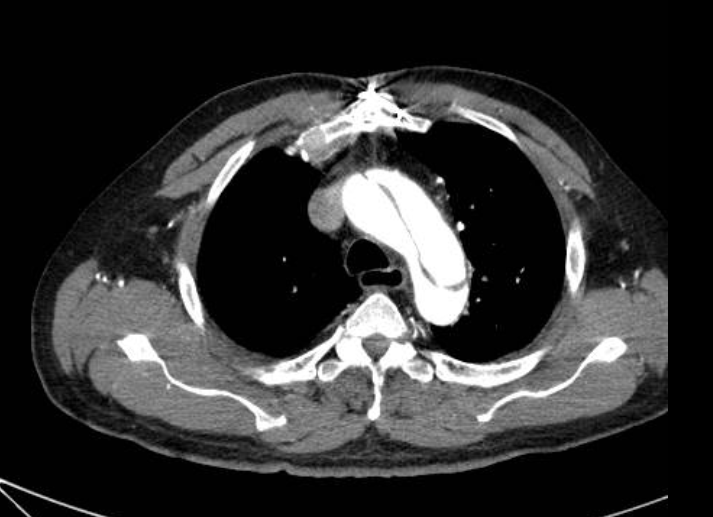
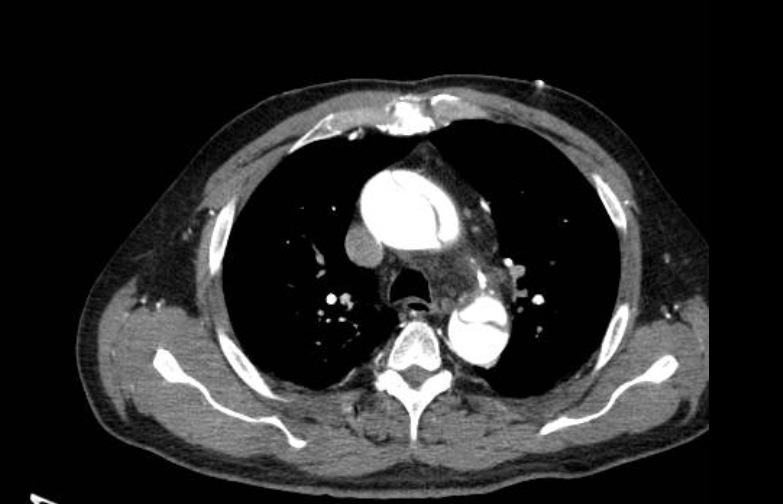
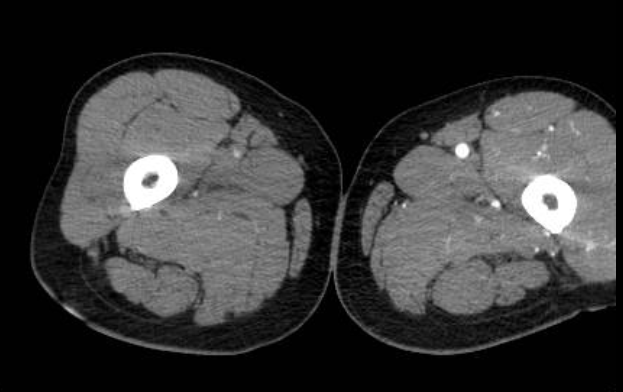
The initial electrocardiogram showed no evidence of acute myocardial infarction. Bedside transthoracic echocardiography demonstrated an intimal flap in the ascending aorta, suggestive of aortic dissection. Computed tomography angiography (CTA) confirmed a Type A aortic dissection extending from the ascending aorta to the iliac bifurcation (Figures 1 and 2), with a thrombus occluding the right popliteal artery (Figure 3). The CTA of the thoracic and abdominal aorta with contrast was performed, and multiplanar and 3D reconstructions were obtained.
Popliteal artery embolism is an uncommon but critical complication of Type A aortic dissection (TAAD), a life-threatening condition that requires immediate intervention. While chest pain is the hallmark symptom of TAAD, the migration of intimal flaps or thrombi into peripheral arteries, such as the popliteal artery, can result in severe limb-threatening complications. This case report aimed to describe an elderly male with a history of hypertension and hyperlipidemia who presented with sudden-onset chest pain and acute ischemia of the right lower extremity due to popliteal artery embolism secondary to TAAD. The case underscored the diagnostic and therapeutic challenges associated with this rare presentation and highlighted the importance of considering TAAD in the differential diagnosis of acute limb ischemia (ALI), particularly in patients with cardiovascular risk factors. Early recognition, prompt imaging, and a multidisciplinary approach to management are essential to improve outcomes in this high-risk population (1,2).
Case
A 72-year-old male with a history of poorly controlled hypertension and hyperlipidemia presented to the Emergency Department with sudden-onset, severe chest pain radiating to his back. He also reported acute-onset pain and coldness in his right lower extremity. Physical examination revealed that he was tachycardic (heart rate: 110 bpm) and hypertensive (blood pressure: 160/100 mmHg). The right lower extremity was pale, cool, and pulseless, with diminished sensation and motor function.
The initial electrocardiogram showed no evidence of acute myocardial infarction. Bedside transthoracic echocardiography demonstrated an intimal flap in the ascending aorta, suggestive of aortic dissection. Computed tomography angiography (CTA) confirmed a Type A aortic dissection extending from the ascending aorta to the iliac bifurcation (Figures 1 and 2), with a thrombus occluding the right popliteal artery (Figure 3). The CTA of the thoracic and abdominal aorta with contrast was performed, and multiplanar and 3D reconstructions were obtained.
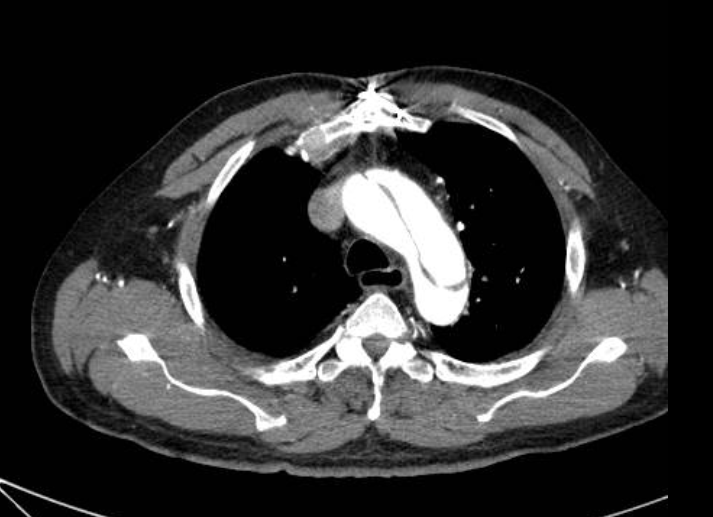
Figure 1. An extensive dissection that was noted from the aortic valve root, ascending aorta, and aortic arch
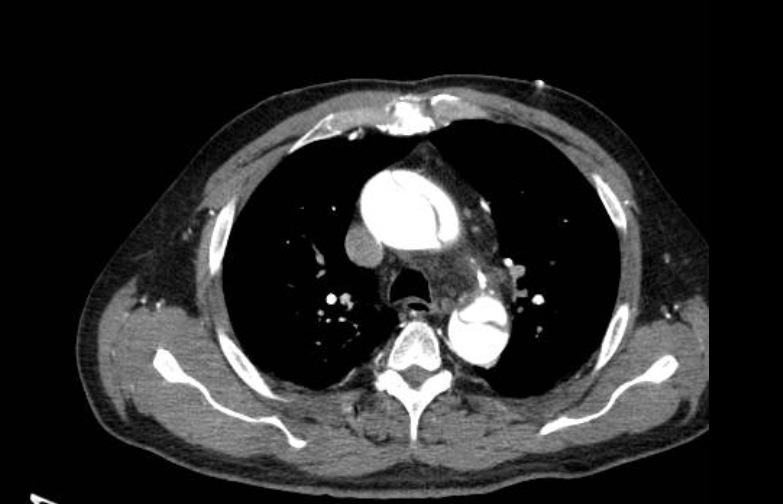
Figure 2. A wide aortic dissection extending to the thoracic aorta and continuing into the abdominal aorta
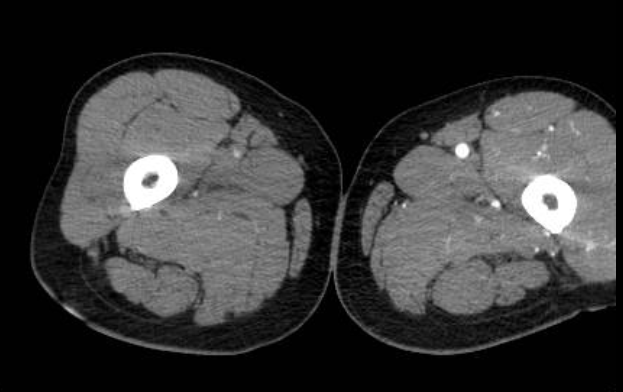
Figure 3. No contrast enhancement visualized in the right popliteal artery, concerning for possible thrombosis or occlusion
The patient was immediately started on intravenous beta-blocker therapy with esmolol to control heart rate and reduce aortic wall stress, targeting a systolic blood pressure between 100-120 mmHg. Nicardipine was added as an intravenous vasodilator to further lower blood pressure after beta-blockade was established. Morphine was administered for pain control to minimize sympathetic stimulation. The ischemic right lower extremity was kept at heart level, and compartment syndrome was monitored through serial clinical examinations. No anticoagulation or thrombolytics were given due to the high risk of aortic rupture. The patient was immediately taken to the operating room for emergent surgical repair of the aortic dissection and thrombectomy of the popliteal artery. Intraoperatively, a large intimal tear was identified in the ascending aorta, and a graft replacement was performed. The popliteal artery was successfully revascularized, and the patient was transferred to the intensive care unit (ICU) postoperatively.
At the three-month visit, the patient underwent a transthoracic echocardiogram to assess aortic valve function and ventricular performance. The previously affected right lower extremity showed improved perfusion, but mild claudication persisted, prompting a referral to supervised physical therapy. A repeat CTA at six months confirmed stable aortic dimensions without evidence of dissection progression or anastomotic complications.
Discussion
The ALI is a vascular emergency characterized by a sudden decrease in limb perfusion, threatening tissue viability. While the most common causes of ALI include arterial thrombosis and embolism from cardiac sources, TAAD is a rare but critical etiology. It should be mentioned that TAAD can lead to malperfusion syndromes, including ALI, due to the migration of intimal flaps or thrombi into peripheral arteries. Incidence of lower extremity malperfusion in TAAD patients is approximately 11% (1).
Pathophysiology involves the formation of an intimal tear in the ascending aorta, which propagates distally and can lead to the detachment of intimal flaps or thrombi. These emboli can occlude peripheral arteries, most commonly the iliac, femoral, or popliteal arteries, resulting in ALI. Severity of ischemia depends on the location and extent of the occlusion, as well as the presence of collateral circulation (2).
Patients with ALI due to TAAD typically present with the classic symptoms of aortic dissection, including sudden-onset and severe chest or back pain, often described as "tearing" or "ripping." Concurrently, they may exhibit signs of ALI, such as pain, pallor, pulselessness, paresthesia, and paralysis in the affected limb. However, the diagnosis can be challenging, as the symptoms of ALI may overshadow or distract from the underlying aortic dissection (3).
Several case reports have highlighted the variability in presentation. For example, a 65-year-old male with TAAD presented with ALI as the primary symptom, with minimal chest pain. In another case, a 58-year-old female with TAAD developed bilateral lower extremity ischemia due to embolic occlusion of the iliac arteries. These cases underscore the importance of considering TAAD in the differential diagnosis of ALI, particularly in patients with risk factors for aortic dissection (4).
Diagnosis of ALI due to TAAD requires a high index of suspicion and a systematic approach. Initial evaluation should include a thorough history and physical examination, focusing on signs of both aortic dissection and limb ischemia. Moreover, imaging plays a crucial role in confirming the diagnosis. The CTA is the gold standard for diagnosing TAAD and identifying the site of arterial occlusion. It provides detailed visualization of the aortic lumen, intimal flap, and peripheral arteries. Transthoracic echocardiography and transesophageal echocardiography are also valuable tools for assessing the ascending aorta and cardiac structures (5).
Despite advances in imaging, diagnostic delays are common. In one case series, the median time from symptom onset to diagnosis was 12 h, highlighting the need for increased awareness and prompt evaluation (6).
Management of ALI due to TAAD requires a multidisciplinary approach, involving cardiothoracic surgery, vascular surgery, and critical care. The primary goals are to address the aortic dissection and restore limb perfusion. Emergent surgical repair of TAAD is the definitive treatment. This typically involves replacing the dissected segment of the aorta with a graft. In cases where ALI is present, aortic repair should be prioritized, as it addresses the source of emboli and prevents further complications. Revascularization of the affected limb can be achieved through surgical thrombectomy, endovascular techniques, or bypass surgery. Choice of intervention depends on the hemodynamic stability of the patient, the extent of ischemia, and the availability of expertise. Anticoagulation and antiplatelet therapy are generally contraindicated in TAAD due to the risk of hemorrhage. However, they may be considered in select cases of ALI after aortic repair (7).
Prognosis of ALI due to TAAD is poor, with reported mortality rates ranging from 20% to 50% (8). Limb salvage rates vary depending on the timeliness of intervention, with earlier revascularization associated with better outcomes. Complications, such as reperfusion injury, compartment syndrome, and multi-organ failure, are common and contribute to the high morbidity and mortality. A case series of 15 patients with ALI due to TAAD has reported a mortality rate of 33%, with limb salvage achieved in 60% of cases. Another study has highlighted the importance of rapid diagnosis and treatment, with a mortality rate of 25% in patients who underwent surgery within 6 h of symptom onset, compared to 50% in those with delayed intervention (9).
Conclusions
The ALI due to TAAD is a rare but devastating complication that requires prompt recognition and management. Clinicians should maintain a high index of suspicion for TAAD in patients presenting with ALI, particularly in the presence of risk factors for aortic dissection. This case highlights the importance of considering aortic dissection in the differential diagnosis of chest pain, particularly in patients with risk factors, such as hypertension. A multidisciplinary approach, involving early imaging, emergent aortic repair, and limb revascularization, is essential to improve outcomes. Further research is needed to optimize diagnostic and therapeutic strategies for this challenging condition.
Conflict of Interest
None to disclose.
At the three-month visit, the patient underwent a transthoracic echocardiogram to assess aortic valve function and ventricular performance. The previously affected right lower extremity showed improved perfusion, but mild claudication persisted, prompting a referral to supervised physical therapy. A repeat CTA at six months confirmed stable aortic dimensions without evidence of dissection progression or anastomotic complications.
Discussion
The ALI is a vascular emergency characterized by a sudden decrease in limb perfusion, threatening tissue viability. While the most common causes of ALI include arterial thrombosis and embolism from cardiac sources, TAAD is a rare but critical etiology. It should be mentioned that TAAD can lead to malperfusion syndromes, including ALI, due to the migration of intimal flaps or thrombi into peripheral arteries. Incidence of lower extremity malperfusion in TAAD patients is approximately 11% (1).
Pathophysiology involves the formation of an intimal tear in the ascending aorta, which propagates distally and can lead to the detachment of intimal flaps or thrombi. These emboli can occlude peripheral arteries, most commonly the iliac, femoral, or popliteal arteries, resulting in ALI. Severity of ischemia depends on the location and extent of the occlusion, as well as the presence of collateral circulation (2).
Patients with ALI due to TAAD typically present with the classic symptoms of aortic dissection, including sudden-onset and severe chest or back pain, often described as "tearing" or "ripping." Concurrently, they may exhibit signs of ALI, such as pain, pallor, pulselessness, paresthesia, and paralysis in the affected limb. However, the diagnosis can be challenging, as the symptoms of ALI may overshadow or distract from the underlying aortic dissection (3).
Several case reports have highlighted the variability in presentation. For example, a 65-year-old male with TAAD presented with ALI as the primary symptom, with minimal chest pain. In another case, a 58-year-old female with TAAD developed bilateral lower extremity ischemia due to embolic occlusion of the iliac arteries. These cases underscore the importance of considering TAAD in the differential diagnosis of ALI, particularly in patients with risk factors for aortic dissection (4).
Diagnosis of ALI due to TAAD requires a high index of suspicion and a systematic approach. Initial evaluation should include a thorough history and physical examination, focusing on signs of both aortic dissection and limb ischemia. Moreover, imaging plays a crucial role in confirming the diagnosis. The CTA is the gold standard for diagnosing TAAD and identifying the site of arterial occlusion. It provides detailed visualization of the aortic lumen, intimal flap, and peripheral arteries. Transthoracic echocardiography and transesophageal echocardiography are also valuable tools for assessing the ascending aorta and cardiac structures (5).
Despite advances in imaging, diagnostic delays are common. In one case series, the median time from symptom onset to diagnosis was 12 h, highlighting the need for increased awareness and prompt evaluation (6).
Management of ALI due to TAAD requires a multidisciplinary approach, involving cardiothoracic surgery, vascular surgery, and critical care. The primary goals are to address the aortic dissection and restore limb perfusion. Emergent surgical repair of TAAD is the definitive treatment. This typically involves replacing the dissected segment of the aorta with a graft. In cases where ALI is present, aortic repair should be prioritized, as it addresses the source of emboli and prevents further complications. Revascularization of the affected limb can be achieved through surgical thrombectomy, endovascular techniques, or bypass surgery. Choice of intervention depends on the hemodynamic stability of the patient, the extent of ischemia, and the availability of expertise. Anticoagulation and antiplatelet therapy are generally contraindicated in TAAD due to the risk of hemorrhage. However, they may be considered in select cases of ALI after aortic repair (7).
Prognosis of ALI due to TAAD is poor, with reported mortality rates ranging from 20% to 50% (8). Limb salvage rates vary depending on the timeliness of intervention, with earlier revascularization associated with better outcomes. Complications, such as reperfusion injury, compartment syndrome, and multi-organ failure, are common and contribute to the high morbidity and mortality. A case series of 15 patients with ALI due to TAAD has reported a mortality rate of 33%, with limb salvage achieved in 60% of cases. Another study has highlighted the importance of rapid diagnosis and treatment, with a mortality rate of 25% in patients who underwent surgery within 6 h of symptom onset, compared to 50% in those with delayed intervention (9).
Conclusions
The ALI due to TAAD is a rare but devastating complication that requires prompt recognition and management. Clinicians should maintain a high index of suspicion for TAAD in patients presenting with ALI, particularly in the presence of risk factors for aortic dissection. This case highlights the importance of considering aortic dissection in the differential diagnosis of chest pain, particularly in patients with risk factors, such as hypertension. A multidisciplinary approach, involving early imaging, emergent aortic repair, and limb revascularization, is essential to improve outcomes. Further research is needed to optimize diagnostic and therapeutic strategies for this challenging condition.
Conflict of Interest
None to disclose.
Type of Study: Case Report |
Subject:
Emergency Medicine
Received: 2025/05/11 | Accepted: 2025/06/24 | ePublished ahead of print: 2025/08/4
Received: 2025/05/11 | Accepted: 2025/06/24 | ePublished ahead of print: 2025/08/4
References
1. Brown JA, Aranda-Michel E, Navid F, Serna-Gallegos D, Thoma F, Sultan I. Outcomes of emergency surgery for acute type A aortic dissection complicated by malperfusion syndrome. J Thorac Cardiovasc Surg. 2024;167(3):882-92. [DOI:10.1016/j.jtcvs.2022.04.051]
2. Sapalo AT. Combined Ultrasound in Screening. In: Smith DL, Johnson RW, editors. Advances in Vascular Surgery: From the Diagnostic Phase to the Use of Hybrid and Endovascular Techniques in the Management of Aortic Dissection. 1st ed. New York: Springer; 2025.
3. Hirao Y, Fujiuchi B, Benavente K, Morihara C, Sakamoto A, Itoga N, et al. Acute Limb Ischemia Presenting as a Clinical Conundrum: Stroke Mimic or Aortic Dissection? European journal of case reports in internal medicine. 2025;12(4):005317. [DOI:10.12890/2025_005317]
4. Patel NN, Kurnick A, Bukharovich I. Atypical presentation of a type a aortic dissection in a patient with an undiagnosed genetic predisposition. Cureus. 2024;16(3):e56394. [DOI:10.7759/cureus.56394]
5. Jaffar-Karballai M, Tran TT, Oremakinde O, Zafar S, Harky A. Malperfusion in acute type A aortic dissection: management strategies. J Vasc Endovasc Surg. 2021;55(7):721-9. [DOI:10.1177/15385744211017116]
6. Bossone E, Eagle KA. Epidemiology and management of aortic disease: aortic aneurysms and acute aortic syndromes. Nat Rev Cardiol. 2021;18(5):331-48. [DOI:10.1038/s41569-020-00472-6]
7. Plotkin A, Vares-Lum D, Magee GA, Han SM, Fleischman F, Rowe VL. Management strategy for lower extremity malperfusion due to acute aortic dissection. J Vasc Surg. 2021;74(4):1143-51. [DOI:10.1016/j.jvs.2021.04.032]
8. Zhang Y, Chen T, Chen Q, Min H, Nan J, Guo Z. Development and evaluation of an early death risk prediction model after acute type A aortic dissection. Ann Transl Med. 2021;9(18):1442. [DOI:10.21037/atm-21-4063]
9. Natour AK, Rteil A, Shepard A, Weaver M, Nypaver T, Nemeh H, et al. Outcomes of patients with acute type A aortic dissection and concomitant lower extremity malperfusion. J Vasc Surg. 2022;76(3):631-8. [DOI:10.1016/j.jvs.2022.03.888]
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |







